Department of Neurosurgery, Xuanwu Hospital 2024-05-26 19:10 Beijing

The “Tuesday Review of Surgery” is a surgical review session for Department of Neurosurgery in Xuanwu Hospital, which has been a long-standing tradition and brand activity of our department. A resident neurosurgeon will introduce each carefully selected surgery with clinical information and play the edited surgical video with key surgical procedures. Then the lead neurosurgeon will summarize the surgical highlights and the surgical team will take questions from the audience around the whole department. In this rigorous and open discussion, fellow neurosurgeons analyze the pros and cons of each case, and learn from each other’s experiences to improve themselves. In order to encourage the continuous pursuit of the perfection of knowledge and techniques, the department upgraded the surgical review session to “Skills of Xuanwu Neurosurgery-New Technique / Complex Surgery / Treatment of critical case” competition. The audience will score each case according to the difficulty, presentation, and discussion. The winning cases will be shared on publicizing platforms such as WeChat public account, YouTube, TikTok and so on. We welcome comments and suggestions from domestic and foreign colleagues!
Difficult cases of "Skills of Xuanwu Neurosurgery" in 2024
-Neuro-Spine Center
Difficult Cases
Scoliosis Growth Rod Orthosis
Operator: Wang Kai
Medical history
A 6-year-old girl
Complaint: Congenital scoliosis deformity, huge skin space-occupying (neurofibroma).
Right lower limb muscle strength grade 4
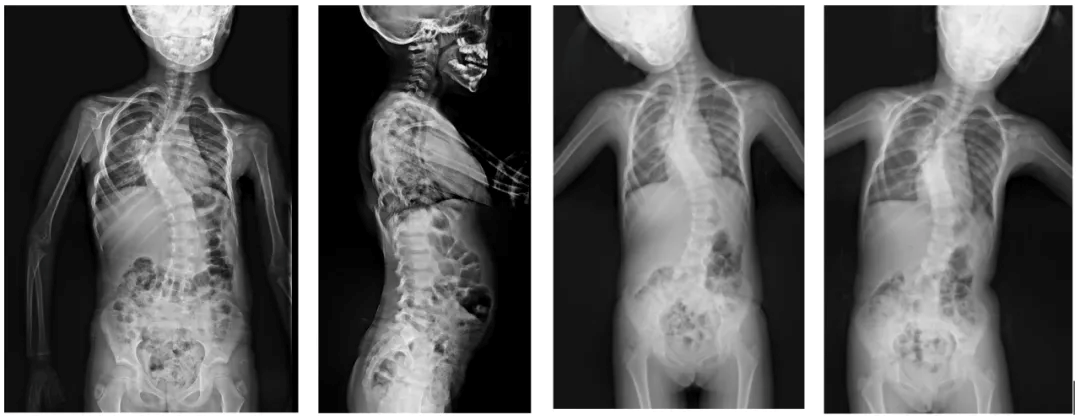
Preoperative imaging examination
2019-05-05: consistent with scoliosis deformity
1. Full-length spine film consistent with scoliosis deformity
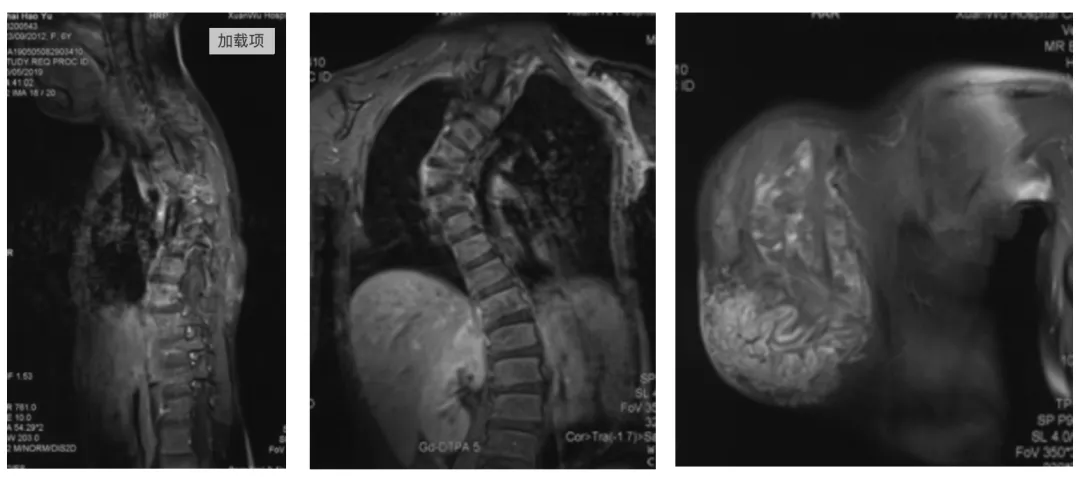
2. Thoracic spine MRI suggesting huge subcutaneous mass with scoliosis
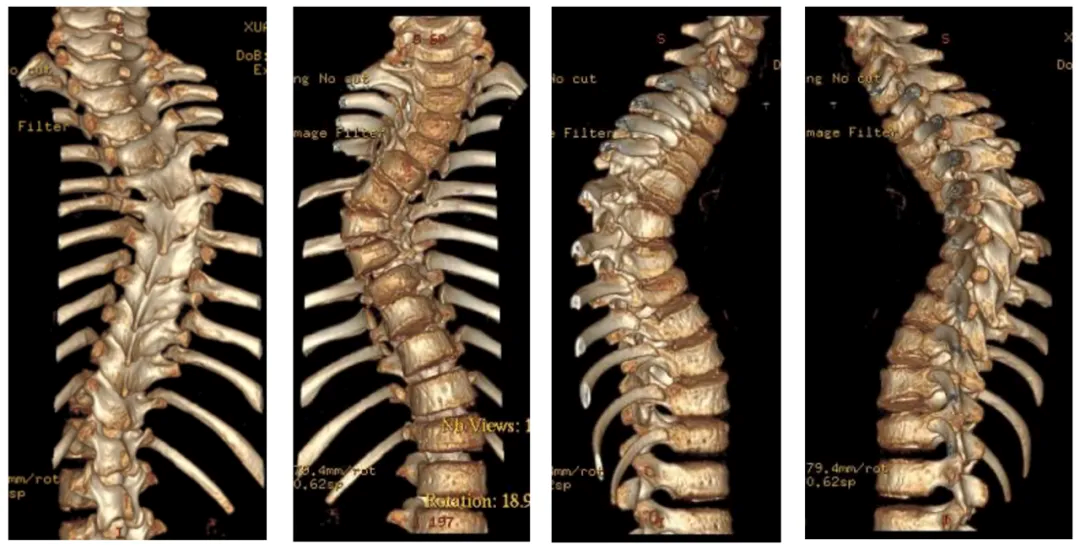
3. CT of thoracic spine showing scoliosis
Preoperative gross view

Diagnosis
Scoliosis deformity, neurofibromatosis
Surgical Procedure
Purpose: To address scoliosis deformity and determine the surgical approach to growth rod to facilitate the adjustment of the child's growth process
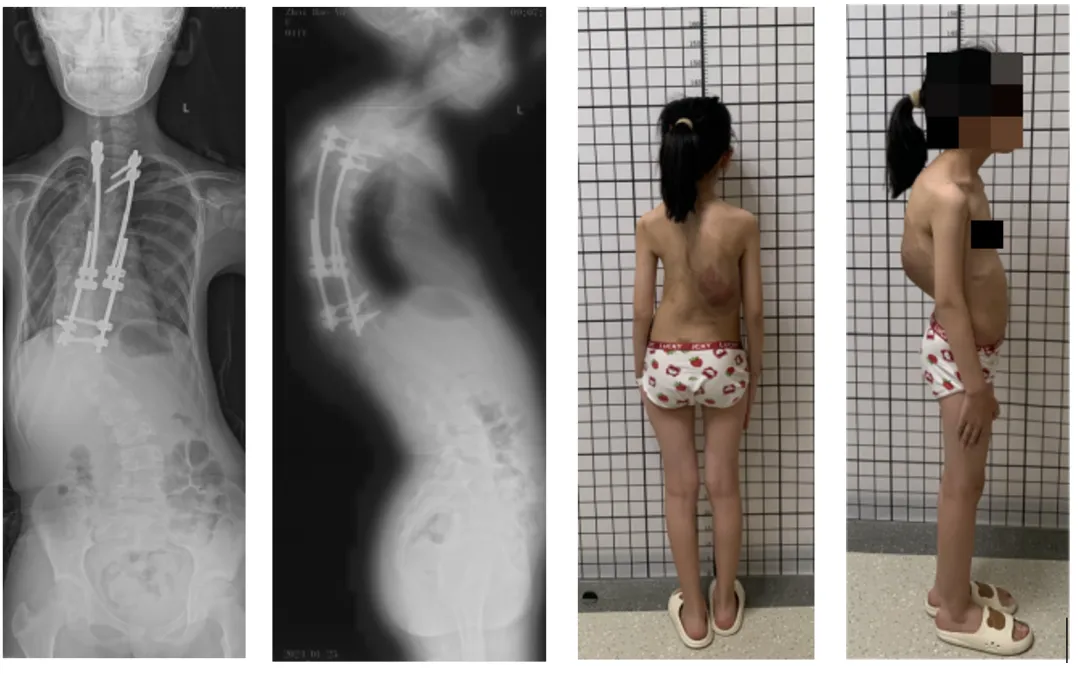
(1) May 10, 2019, growth rod implantation, pre- and post-operative comparisons

(2) 2020-01-15, the first growth rod adjustment: left concave side braced 1.5cm; right convex side braced 1.2cm;
(3) 2020-07-23, the second growth rod adjustment: left concave side stretched 1.5cm; right convex side stretched 1.2cm;
(4) 2021-03-26, the third growth rod adjustment: left concave side propped open 1.5cm; right convex side propped open 1.0cm;
(5) 2021-10-14, the fourth growth rod adjustment: left concave side stretched 1.0cm; right convex side stretched 0.5cm;
(6) 2022-05-22, the fifth growth rod adjustment: bilaterally propped open 1.0cm;
(7) 2023-01-11, both sides were stretched 1.0cm, and one domino on each side was added;
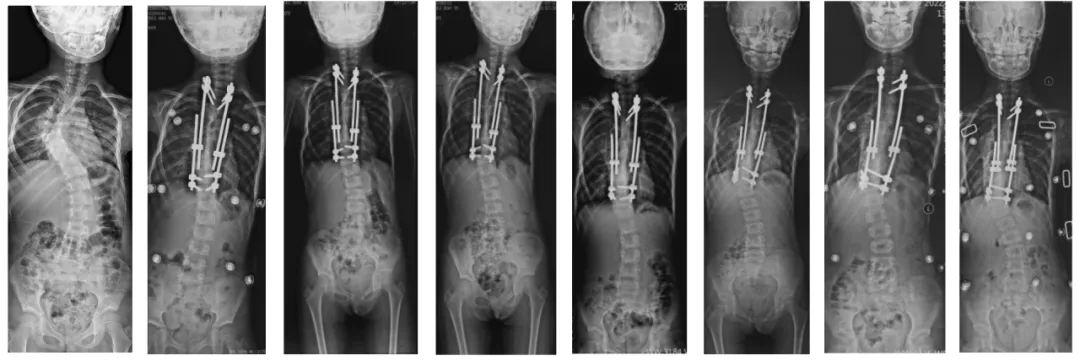
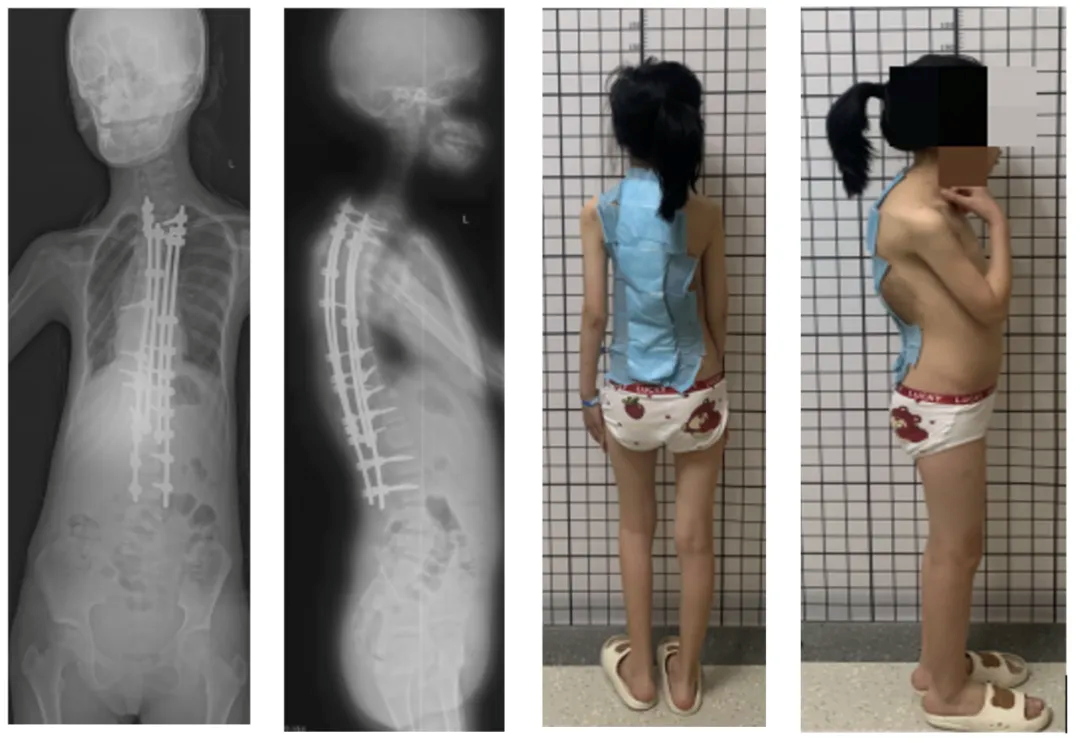
Preoperative → growth rod implantation → full-length piece orthotopic after 6 adjustments
Revision surgery
2024-01-30: aggravation of scoliosis deformity
Surgical procedure
(1) The original straight incision in the posterior median was taken and extended downward (about 30 cm) to the T2-L3 level.
(2) Part of the subcutaneous tumor was sent for pathology;
(3) O-arm fluoroscopy was used to implant bilateral pedicle screws at T9 and T12-L3, right pedicle screw at T7, and new pedicle screws at T2-3 and T10-11, but the remaining pedicles were not able to be implanted due to dysplasia;
(4) Fluoroscopy showed satisfactory screw position and temporary rod fixation. Ultrasonic bone knife was used to remove the T12-L3 vertebral plate and inferior articular process. The upper rod is slightly compressed on the left side and slightly braced on the right side;
(5) In-situ locking screws, C-arm fluoroscopy shows satisfactory position of the nail-rod system.
Postoperative images
Postoperative MRI + enhancement
Postoperative pathology
Neurofibroma type 1 was considered. Immunohistochemistry and special staining results:
(1) SOX-10 (-), S100 (-), NF (-), CD34 (diffuse + ), Ki-67 (~2% +); reticulofibrillar (+ ),AB/PAS (AB +).
(Patient information is for professional discussion only with the consent of the patient and his family)
Operator's comment
The treatment of NF1-associated scoliosis remains debated, and it is relatively clear that brace therapy is ineffective, progresses rapidly, and surgical intervention is recommended. Younger patients (usually under 10 years) are treated with the growth rod technique.
Determining a reasonable fixation segment is a key component in spinal deformity surgery for neurofibromatosis. The selection of the fixation segment requires comprehensive consideration of the following aspects:
(1) Type and extent of deformity
According to the type of deformity (scoliosis, kyphosis, etc.) and the range of the affected segments, the main curvature to be corrected should be determined. Usually, it is necessary to fix 2-4 segments above and below the curved segments to reach the neutral vertebrae.
(2) Bone condition
Since neurofibromatosis is often accompanied by osteoporosis, orthopedics may involve the extraction of nails and the risk of implant failure, which need to be paid attention to when orthopedics.
(3) Tumor infiltration
If there is tumor infiltration in some segments or important neurovascular structures are endangered, these areas should be avoided.
(4) Patient's age and activity requirements
Older patients or patients with lower activity requirements may choose relatively short fixed segments. Younger, more active patients require longer fixation segments to achieve adequate stability.
Taking all of these factors into consideration, the neurosurgical and spinal teams will usually determine the optimal fixation segment during the preoperative evaluation. Adjustments may also be made during the surgery, depending on the actual situation. The general principle is to balance the orthopedic needs with the risk of complications in order to achieve the best possible outcome.
In this case, the child showed rapid distal progression after several rod adjustments, and therefore required prompt surgical correction. Due to the limited growth potential of the child as he approached puberty, a lengthening segmental orthosis with terminal fusion was considered as an option.

Group photo of Neuro-Spine Center
Introduction of surgeon

Wang Kai
Department of Neurosurgery, Xuanwu Hospital, Capital Medical University
Neuro-Spine Center
Consultant Neurosurgeon
MD. PhD.
Dr. Wang graduated from Peking Union Medical College and received his PhD degree in Orthopedics under the supervision of Academician Qiu Guixing.
He has profound attainments in minimally invasive treatment of age-related degenerative spine diseases, neck, shoulder, back and leg pain and scoliosis. He is a young lecturer of AO Spine, a young member of SICOT China Division, and a young member of Spinal Cord Committee of China Research Hospital Association (CRHA/NSAC).
Specialties: minimally invasive treatment of spinal cord diseases, including the application of microscopic neurosurgical techniques for the minimally invasive treatment of cervical spondylosis, lumbar intervertebral disc herniation, lumbar spinal stenosis, scoliosis deformity, spinal cord tumors, Chiari Malforamtion, atlantoaxial dislocation vertebral subluxation, syringomyelia, and spinal cord tethering.
Clinic Hours: Thursday morning (Specialist Clinic).
Any use of this site constitutes your agreement to the Terms and Conditions and Privacy Policy linked below.
A single copy of these materials may be reprinted for noncommercial personal use only. "China-INI," "chinaini.org" are trademarks of China International Neuroscience Institute.
© 2008-2021 China International Neuroscience Institute (China-INI). All rights reserved.