Original Department of Neurosurgery, Xuanwu Hospital 2024-04-18 18:02 Beijing
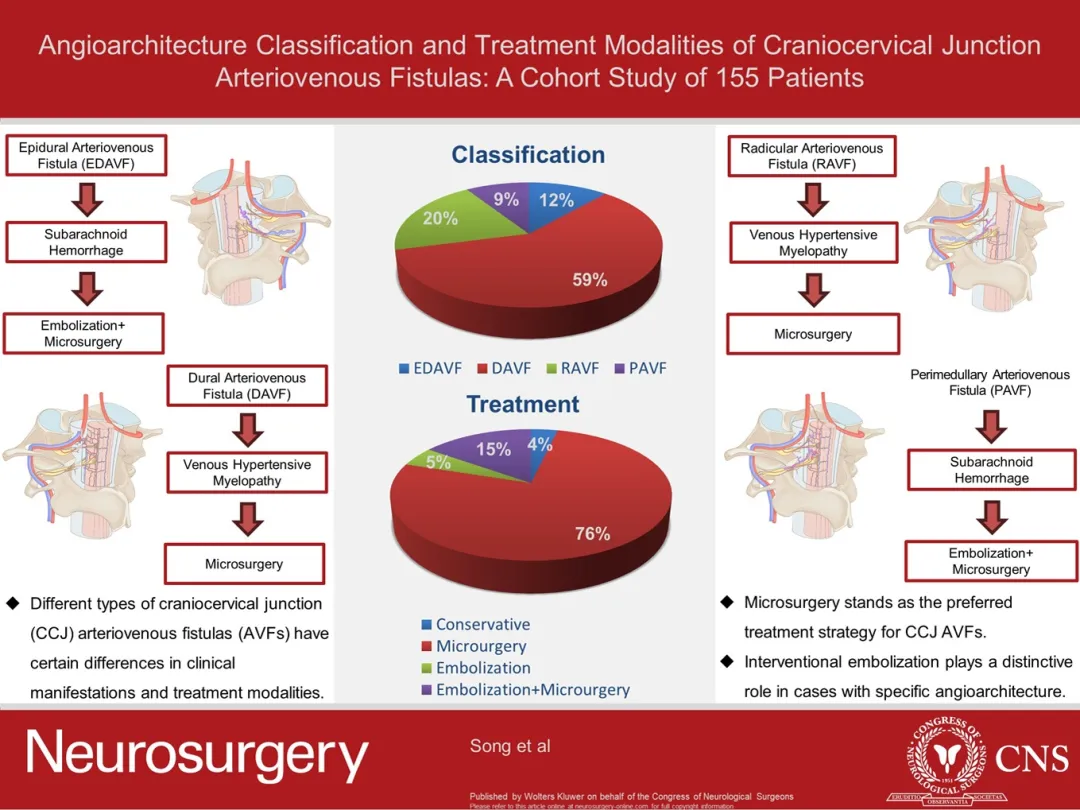
Recently, Prof. Zhang Hongqi's team from the Department of Neurosurgery, Xuanwu Hospital, Capital Medical University, published a paper entitled "Angioarchitecture Classification and Treatment Modalities of Craniocervical Junction Arteriovenous Fistulas: A Cohort Study of 155 Patients". Dr. Song Zihao, Dr. Ma Yongjie, and Dr. Tu Tianqi from the Department of Neurosurgery at Xuanwu Hospital were the co-first authors of the paper, and Prof. Ye Ming and Prof. Zhang Hongqi from the Department of Neurosurgery at Xuanwu Hospital of Capital Medical University were the corresponding authors.
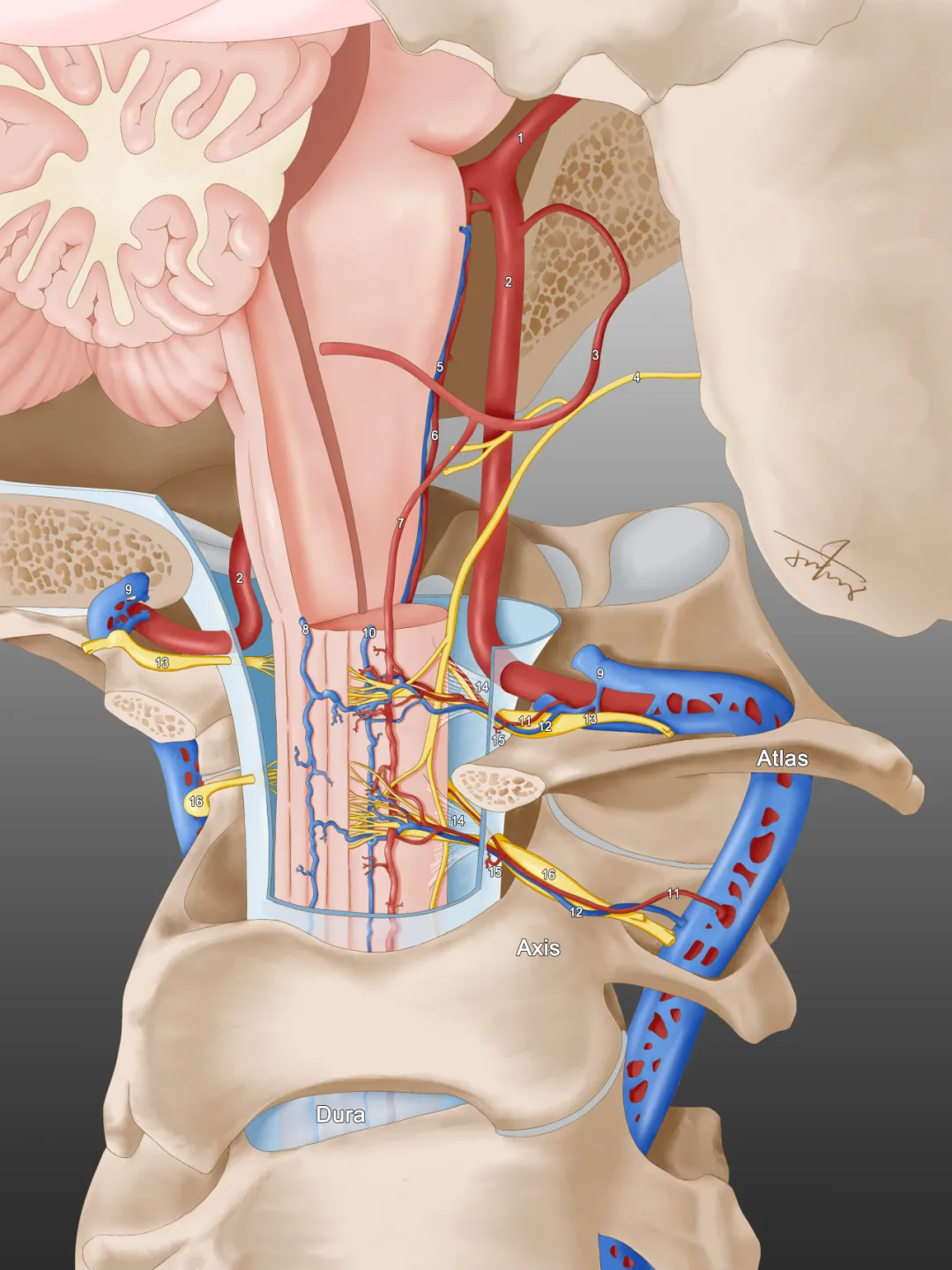
Schematic anatomy of the craniocervical junction region. (1) basilar artery, (2) vertebral artery, (3) posterior inferior cerebellar artery, (4) parasympathetic nerves, (5) anterior median vein of the spinal cord, (6) anterior spinal artery, (7) lateral spinal arteries, (8) posterior median vein of the spinal cord, (9) paravertebral venous plexus, (10) posterior lateral vein of the spinal cord, (11) root artery of the nerves, (12) root veins of the nerves, (13) cervical nerve root of cervical 1, (14) dentate ligament, (15) dural branch of the vertebral artery, and (16) cervical 2 nerve root.
Craniocervical Junction Arteriovenous Fistulas (CCJ AVF)) is a rare arteriovenous fistula accounting for approximately 2% of cerebral and spinal vascular malformations, and due to the unique vascular configuration of CCJ AVF, there are significant differences in clinical symptoms and treatment modalities when compared to Cognard V dural arteriovenous fistula and thoracolumbar dural arteriovenous fistula.
In this study, a total of 155 patients with CCJ AVF who were definitively diagnosed and treated by angiography at the Department of Neurosurgery, Xuanwu Hospital, from January 2012 to December 2021 (165 cases of CCJ AVF) were retrospectively included. CCJ AVF was categorized into 4 types according to the location of the fistula: epidural arteriovenous fistula (EDAVF) (19 cases [11.5%]), dural-type arteriovenous fistula (DAVF) (98 cases [59.4%]), radicular-type arteriovenous fistula (RAVF) (33 cases [20.0%]), and perimedullary-type arteriovenous fistula (PAVF) (15 cases [9.1%]), and re further categorized according to the presence or absence of concomitant cartilaginous arterial supply.
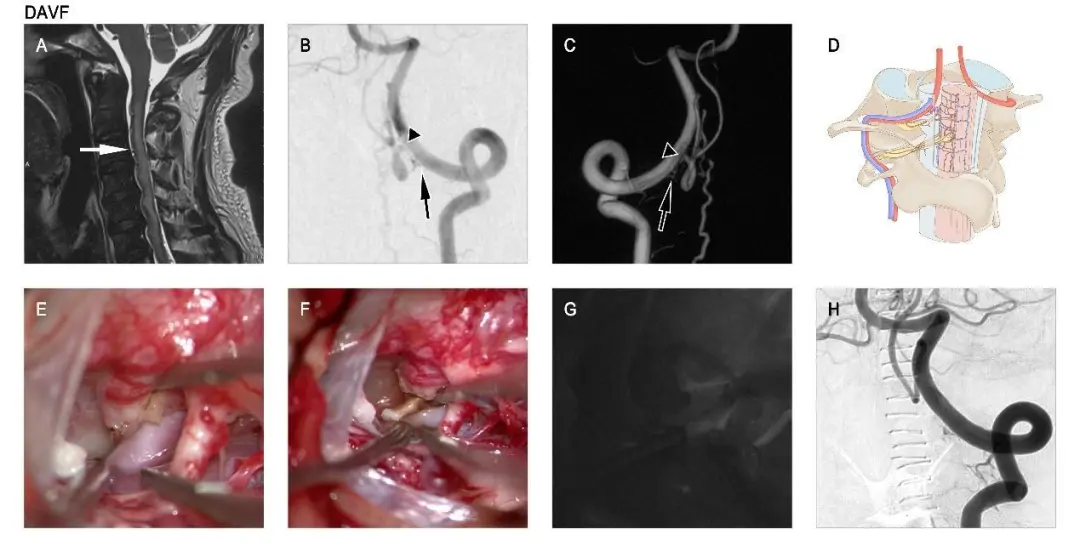
A male with CCJ DAVF patient started with venous hypertensive myelopathy and underwent microsurgery. T2-weighted sagittal MRI image (A) shows cervical medullary high signal and flow-vessel shadows (white arrows in A). Preoperative angiography of the left vertebral artery (B and C). This AVF is supplied by the dural branch of the left C-1 vertebral artery (black arrow in B and C), which drains into the intradural vein (black triangle in B and C). Schematic diagram of the AVF (D) vascular configuration. Intraoperative image showing the AVF and draining vein (E). Intraoperative images and ICG fluorescence angiography show the AVF (F and G) severed. Left vertebral artery angiography at 4 days postoperatively (H).
Overall the most common location of onset in CCJ AVF is at the C-1 level, whereas EDAVF and PAVF in more commonly develop at the C-2 level. In this study, male patients predominated, with a total of 138 (83.6%) CCJ AVFs being male. DAVF mainly started as venous hypertensive myelopathy, while other types of CCJ AVFs often started as subarachnoid hemorrhage. In the treatment of CCJ AVF, the preferred therapeutic strategy is microsurgery, whereas interventional embolization can be used for the treatment of CCJ AVF in specific vascular constructs or to embolize part of the vascular malformation where surgical exposure is difficult before microsurgery.
Any use of this site constitutes your agreement to the Terms and Conditions and Privacy Policy linked below.
A single copy of these materials may be reprinted for noncommercial personal use only. "China-INI," "chinaini.org" are trademarks of China International Neuroscience Institute.
© 2008-2021 China International Neuroscience Institute (China-INI). All rights reserved.