Department of Neurosurgery, Xuanwu Hospital 2024-01-29 18:00 Beijing

The “Tuesday Review of Surgery” is a surgical review session for Department of Neurosurgery in Xuanwu Hospital, which has been a long-standing tradition and brand activity of our department. A resident neurosurgeon will introduce each carefully selected surgery with clinical information and play the edited surgical video with key surgical procedures. Then the lead neurosurgeon will summarize the surgical highlights and the surgical team will take questions from the audience around the whole department. In this rigorous and open discussion, fellow neurosurgeons analyze the pros and cons of each case, and learn from each other’s experiences to improve themselves. In order to encourage the continuous pursuit of the perfection of knowledge and techniques, the department upgraded the surgical review session to “Skills of Xuanwu Neurosurgery-New Technique / Complex Surgery / Treatment of critical case” competition. The audience will score each case according to the difficulty, presentation, and discussion. The winning cases will be shared on publicizing platforms such as WeChat public account, YouTube, TikTok and so on. We welcome comments and suggestions from domestic and foreign colleagues!
Difficult cases of "Xuanwu Technology" in 2024
-Skull Base and Brain Tumor Center
Difficult Cases
Resection of recurrent malignant meningioma in the saddle region by internal carotid artery middle cerebral artery bypass grafting.
Operators: Xiao Xinru, Hu Peng, Bai Jie
Medical history
Female, 51 years oldComplaint: Malignant meningioma in the saddle region recurred 15 years after surgery.In the past 15 years, she underwent 4 craniotomies and 1 gamma knife treatment.Physical examination: clear speech, clear and coherent answers; right eyelid ptosis, photopic vision, temporal hemianopsia, pupil 5mm, loss of light reaction, limited four-way eye movement; left eye vision 0.3, pupil diameter 2mm, sensitive light reaction, normal four-way movement. The muscle strength and tone of the limbs were normal, physiologic reflexes were present, and pathologic reflexes were not elicited.
Preoperative imaging examination
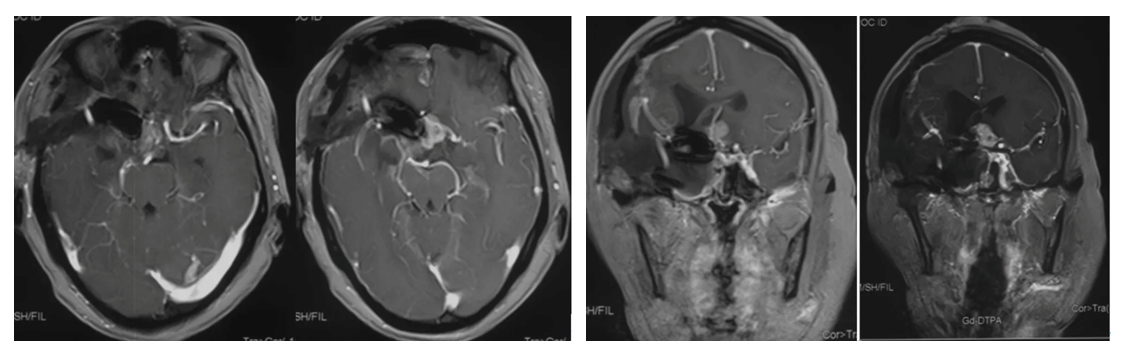
Cranial MRI enhanced
1. MRI T1 and T2 images showed a tumor in the left saddle region with long T1 and short T2 signals. The tumor was solid and encircled the internal carotid artery and branch vessels.
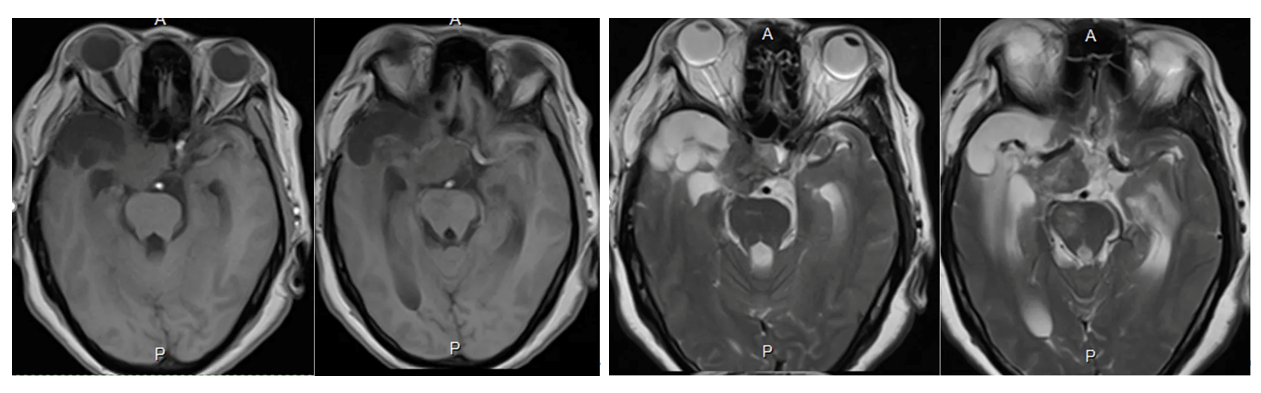
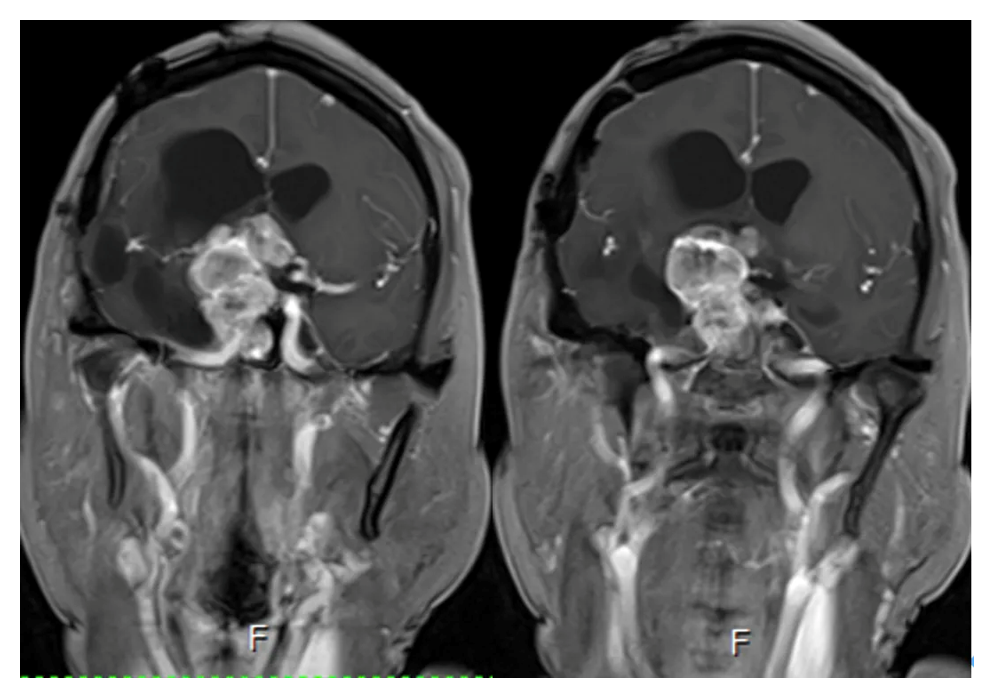
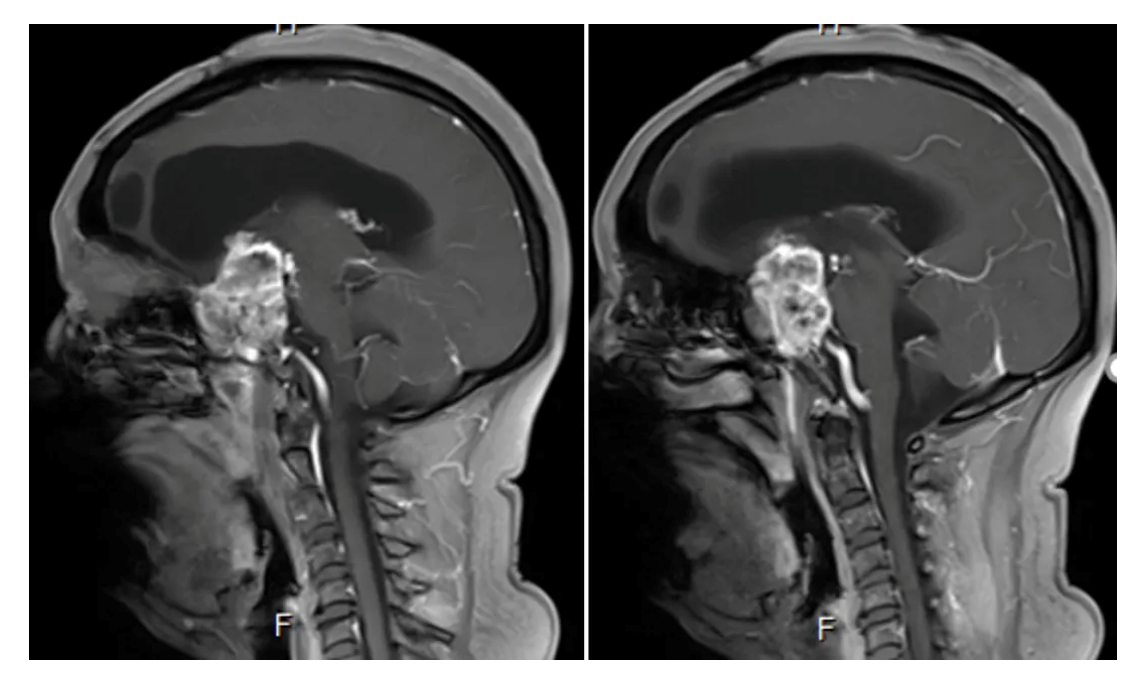
2. Enhanced axial and coronal-sagittal views showed that the tumor was unevenly enhanced, which was located in the saddle region, invaded the right cavernous sinus, and encircled the internal carotid artery and its branches and perforating vessels.
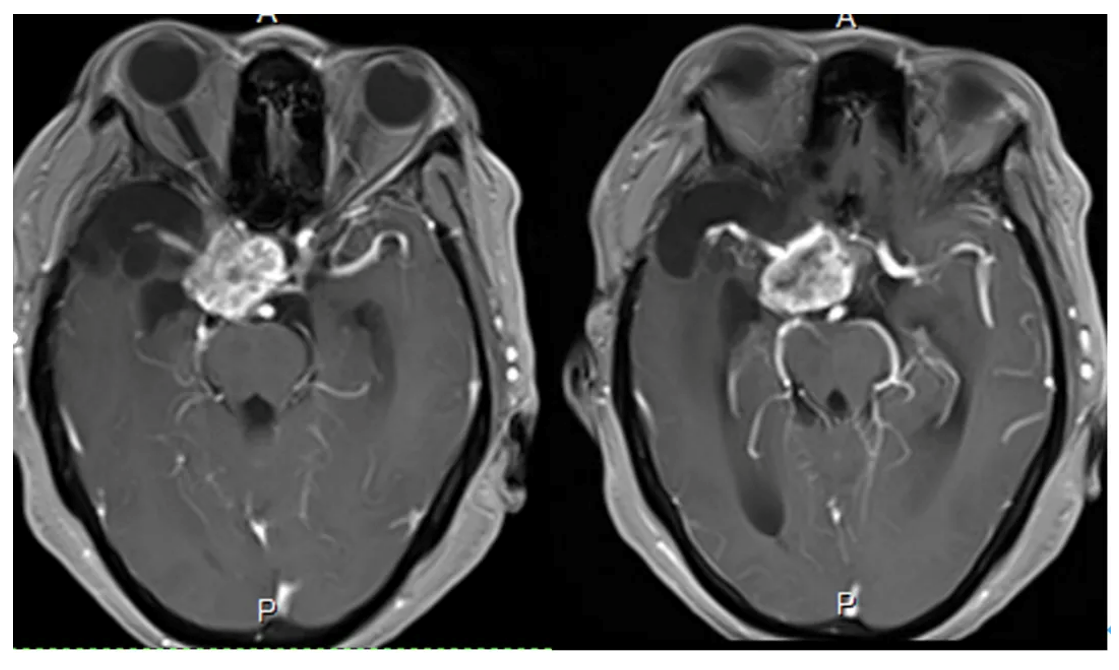
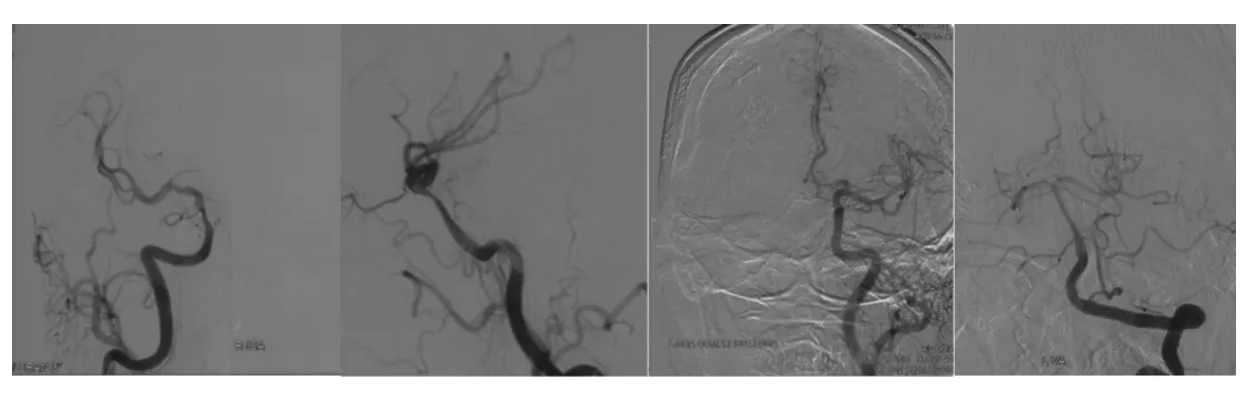
3. Cerebral angiography showed that the right internal carotid artery was unevenly narrowed at the bed-surge segment and the upper end of the bed-surge, displaced medially and superiorly, with the posterior and anterior communications not open, and the middle cerebral artery blood-supplying region had a lesser distribution of blood vessels; the vertebral basilar artery did not have an obvious cortical anastomosis supplying blood to the right cerebral hemisphere; and the left anterior cerebral artery was double-trunked.
Diagnosis:
Recurrent malignant meningioma in the saddle region.
Preoperative discussion
The right saddle region was occupied and recurred many times, also treated by Gamma Knifewith residual regrowth of the tumor. Preoperatively, the right motor nerve was completely paralyzed and had poor vision, but the left limb movement was not affected. Previous pathology had confirmed the diagnosis of malignant meningioma. Taking the above considerations into account, the indications for surgery were clear. How to resect the tumor as much as possible and at the same time protect the blood supply of the branches of the internal carotid artery and the perforating blood vessels was the key to the surgery. The patient had undergone multiple surgeries and radiation treatments in the past, and the tumor was generally hard and tough with severe adhesions, which made it difficult to resect the tumor while protecting the blood vessels. Cerebral angiography showed poor blood supply in the region of the right middle cerebral artery and no good blood supply compensation. Therefore, ensuring the blood supply of the right internal carotid artery is the key to preventing postoperative cerebral infarction, guaranteeing limb survival, and removing the tumor as much as possible. Given that the patient's right superficial temporal artery has been destroyed in many operations, low-flow bypass is not good to realize. Therefore, we considered choosing the radial artery as the bridging vessel to perform high-flow bypass with anastomosis between the internal carotid artery and the middle cerebral artery. While resecting the tumor as much as possible, it is also necessary to protect the internal carotid artery, the anterior cerebral artery and the middle cerebral artery to avoid deep brain infarction. The residual tumor will be treated with adjuvant therapy at a later stage to control the growth.
Treatment strategy
Internal carotid artery middle cerebral artery bypass grafting (radial artery is the bridging vessel) Recurrent malignant meningioma resection.
Adjuvant measures: bilateral radial artery Allen test, electrophysiologic testing including SEP and MEP; intraoperative vascular ultrasound; fluoroscopy; vascular bypass instrumentation
Surgical position: supine position was adopted, and the radial artery was taken by abduction of the right upper limb.
Surgical procedure and details
After fixing the head position with a metal head frame, routinely sterilizing the frontotemporal surgical area and the right upper limb, and laying a sterile sheet, the original incision of the right frontotemporal was incised and the original bone flap was removed. The bone at the base of the middle cranial fossa was smoothed. The dura mater was cut in an arc. Adhesion of the original dura mater to the surface of the brain tissue was seen and separation was given. Right temporal lobe cerebral softening foci were seen with tumor tissue located in the saddle region growing toward the base of the middle cranial fossa and cavernous sinus. The lateral fissure was separated to expose the M2 and M3 branches, and the M1 segment was completely encapsulated by the tumor. The distal end of M2 supplying blood to the frontoparietal was selected as the recipient vessel. Then the bone of the petrous bone was abraded to expose the petrous horizontal segment of the internal carotid artery as the blood-supplying vessel. The right radial artery 15 cm was taken under the microscope as the bridge vessel, trimmed, and the bridge vessel was anastomosed with the internal carotid artery and the middle cerebral artery end to end, respectively. After successful anastomosis, fluorescent imaging showed that the anastomosis was patent and the distal M2 vessels were well visualized. The lateral fissure was continued to be isolated under the microscope to expose the superior segment of the bed process of the internal carotid artery, and clamping was given. Then dissociate the tumor located in the anterior bed protrusion, the base of the middle cranial fossa floor, and resect the tumor in pieces, the tumor was reddish brown, hard and tough, encircling the internal carotid artery, M1 and A1 perforating vessels, and it could not be completely resected. The tumor was resected in large part under microscope. The operation area was strictly hemostatic, the dura mater was sutured, the bone flap was repositioned and fixed, the scalp was sutured layer by layer, and the operation was finished. After removing the metal head frame, the patient returned to ICU with tracheal intubation. 12 hours later, the patient's spontaneous respiration was restored, he was conscious, the trachea was removed, and he could answer correctly and move his limbs voluntarily.
In this case of meningioma patient, vascular bypass was performed first, and then the tumor was resected to remove as much tumor as possible while ensuring normal blood supply to the brain. In order to preserve the perforating blood vessels, a small amount of tumor was left behind, and the effect of later adjuvant therapy would be better after the tumor volume was significantly reduced.
Pathologic diagnosis
Small cell undifferentiated sarcoma
Postoperative review
Postoperative MRI enhancement: Showing a major resection of the tumor
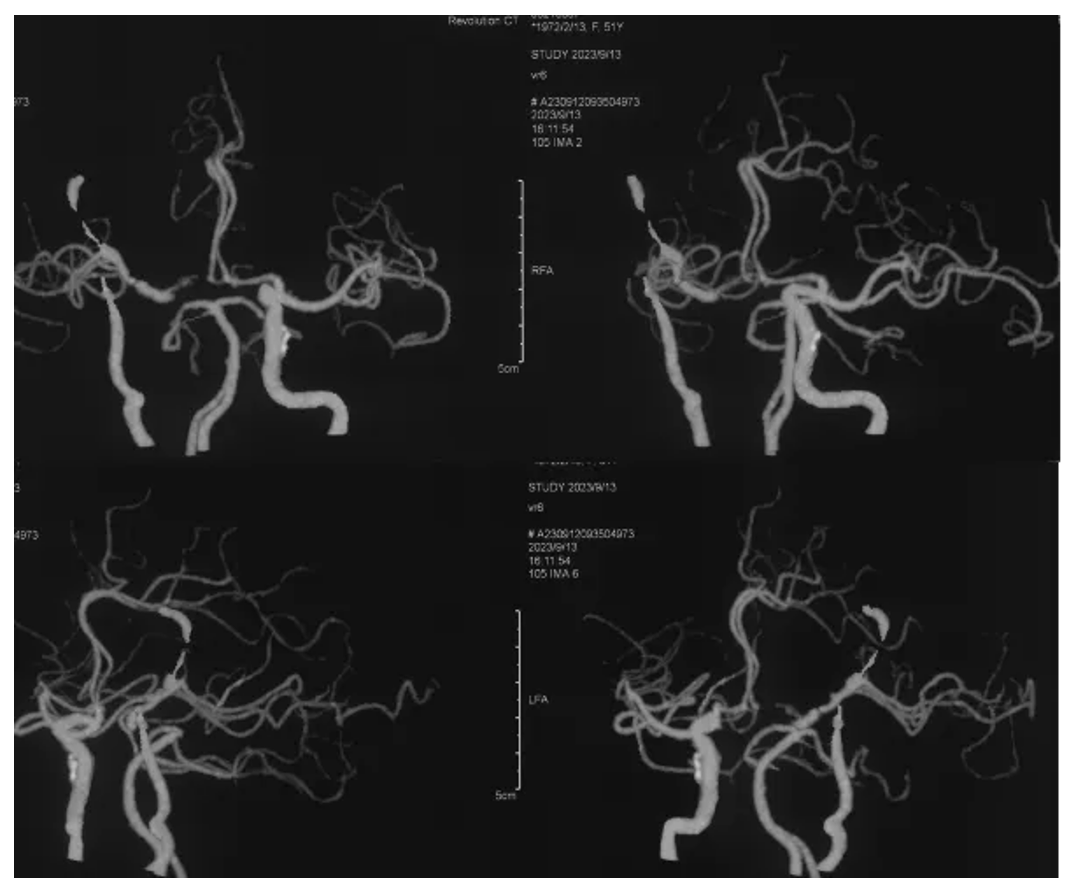
Postoperative CTA
Bridging vascular patency
Postoperative limb movement

(Patient information is for professional discussion only with the consent of the patient and his family)
Operator's comment: "Meningiomas account for about 20% of intracranial tumors
Meningiomas account for about 20% of intracranial tumors, of which 5% to 7% are mesenchymal meningiomas and l% to 3% are malignant meningiomas. Malignant meningiomas are characterized by high aggressiveness, easy recurrence, and poor prognosis, with 5-year and 10-year survival rates of about 65% and 50%, respectively. Currently, surgical resection and postoperative radiotherapy are still the first choice for the treatment of malignant meningiomas. Due to the high recurrence of malignant meningiomas, the initial surgery should strive to achieve total resection, but if the tumor is located in an important functional area, attention needs to be paid to preserving neurological function when removing the tumor. The saddle region is also one of the most common sites for meningiomas. The region has a complex structure, with the internal carotid artery and its branches emanating from the perforating arteries, which supply the blood supply to the basal ganglia region, and serious neurological dysfunction will occur if the injury occurs, which makes the surgery more difficult. Especially in this case, the patient had been operated many times and treated with Gamma Knife, the tumor was hard and tough, with heavy adhesion, encircling the internal carotid artery and the perforating blood vessels, and there was no arachnoid space between the tumor and the blood vessels. The tumor could not be completely resected, and only as much as possible tumor reduction could be done. The tumor can only be decomposed as much as possible to provide good conditions for subsequent auxiliary treatment. The Department of Neurosurgery of Xuanwu Hospital has rich experience in the treatment of various intracranial meningiomas, including convex, skull base, intraventricular, cranial-orbital communicating, and intracranial and extracranial sulcus. According to the characteristics of the tumor, surgery can be performed by microscope, neuroendoscopy or microscope combined with endoscopy, etc. At the same time, neurosurgical robots, navigation, intraoperative nuclear magnetism and other advanced technological means are applied, so as to maximize the resection of the tumor under the premise of protecting neurological function as much as possible.
The annual volume of neurosurgery of Xuanwu Hospital for meningiomas is nearly 1,000, especially for some skull base, deep, huge and recurrent meningiomas, which have accumulated a large number of clinical cases. We will do our best to help every patient to get rid of the diseaseAs long as doctors and patients are of one mind and in the same boat, we will overcome the difficulties.
Group photo of Skull Base and Brain Tumor Center
Any use of this site constitutes your agreement to the Terms and Conditions and Privacy Policy linked below.
A single copy of these materials may be reprinted for noncommercial personal use only. "China-INI," "chinaini.org" are trademarks of China International Neuroscience Institute.
© 2008-2021 China International Neuroscience Institute (China-INI). All rights reserved.