Wang Y, Ma Y, Song Z, Yang C, Tu T, Yang K, He C, Li G, Hu P, Sun L, Ye M, Zhang H. Clinical and prognostic features of venous hypertensive myelopathy from craniocervical arteriovenous fistulas: a retrospective cohort study. J Neurosurg. 2023 Jan 13:1-11. doi: 10.3171/2022.11.JNS221958. Epub ahead of print. PMID: 36640099.
Background of the study
Venous hypertensive myelopathy (VHM) is usually caused by spinal arteriovenous fistulas (SAVF), especially dural arteriovenous fistulas (SDAVF). Several cohort studies have shown that the thoracolumbar spinal cord is the most commonly affected site of SDAVF. However, recognition and treatment of craniocervical junctional area arteriovenous fistulas (CCJAVF) starting with VHM is essential. Several case series of CCJAVF leading to VHM (CCJVHM) have been reported, and unique presentations involving brainstem and upper limb function have been identified. They share the same pathological mechanisms but have different clinical features due to the different lesion locations. The means of neurological function evaluation and long-term prognosis of CCJVHM are currently unclear. This study is a single-center retrospective cohort study of CCJVHM, which will improve the understanding of the means of neurological function evaluation and long-term prognosis of VHM.
Methodology
CCJAVF was defined as a subdural, dural, or epidural arteriovenous fistula located at the level of the jugular foramen, subungual neural canal, greater occipital foramen, and C1 or C2 vertebrae, without intramedullary vascular malformation-like structures. Inclusion criteria for patients with CCJVHM were as follows: 1) Digital Subtraction Angiography (DSA) showing fistula drainage to the surface of the spinal cord or medulla oblongata (ii) high signal on T2 MRI of the spinal cord or medulla oblongata; (iii) clinical manifestations of limb weakness and bowel dysfunction. The DSA findings are required and the other two are optional. The exclusion criteria were as follows: ① CT or MRI examination suggested a hemorrhagic lesion, or the medical history suggested the possibility of hemorrhage (e.g., sudden unbearable pain); ② MRI showed huge dilatation of the draining veins compressing the spinal cord or nerve roots; ③ clinical manifestations were simple pulsatile tinnitus, headache, dizziness and cranial nerve palsy without evidence of spinal cord and medulla oblongata edema. AVF was classified as DAVF, RAVF, EDAVF, and PAVF. all patients were assessed for neurological function at admission and completed by telephone or outpatient follow-up at 7 days, 1 year, 3 years, 5 years, and 7 years postoperatively. All patients underwent MRI or DSA review at 7 days and 1 year postoperatively. Follow-up physicians changed annually and were unaware of previous follow-up records. The study was approved by the Ethics Committee of Xuanwu Hospital, and all patients signed an informed consent form.
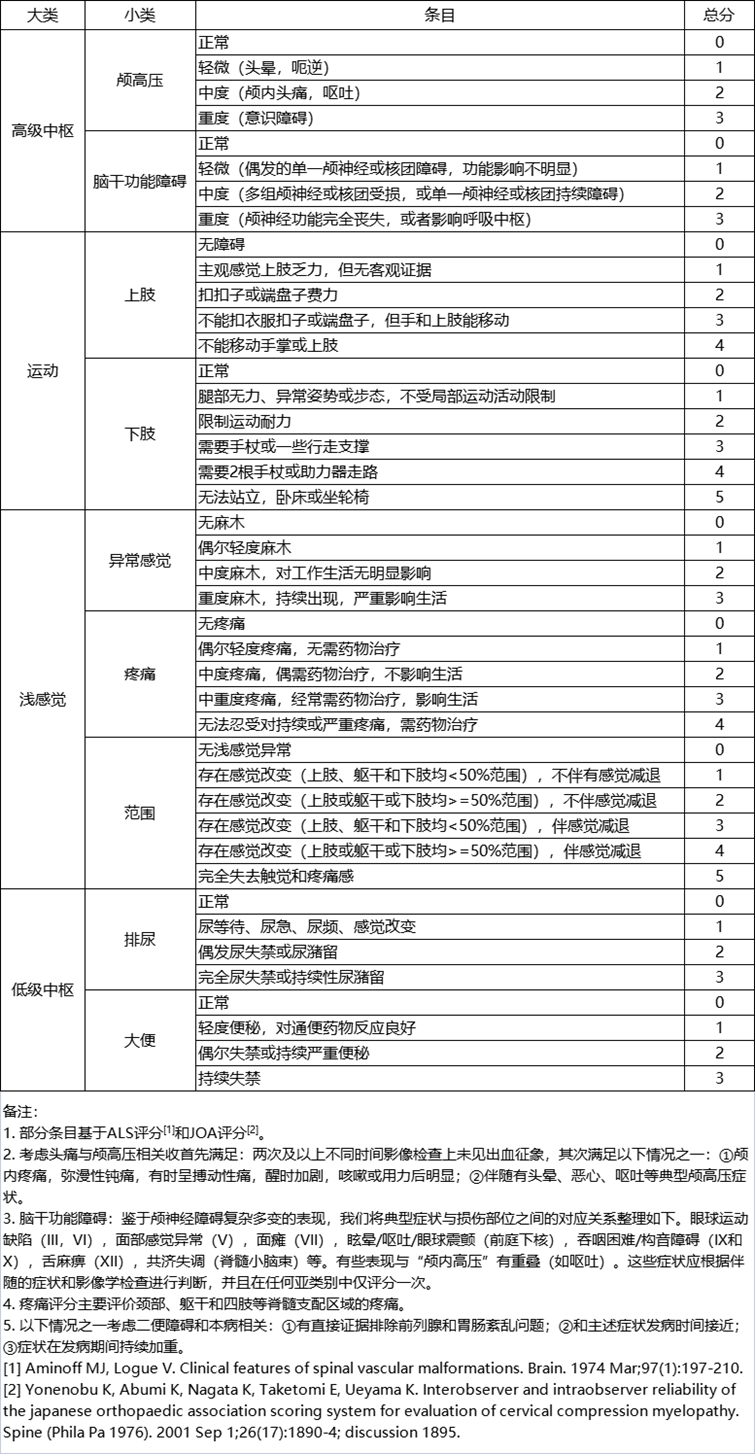
The primary outcome was the patient's improvement in neurological function. Three scales, ALS, JOA, and VHMS, were used to assess each of them. vHMS was developed based on the patient's clinical presentation and physical examination and was partially based on ALS (lower extremity function, urination, and defecation) and JOA (upper extremity and sensory function) criteria. Detailed VHMS score entries are listed in Table 1. Neurological Improvement Rate (NIR) = [(preoperative score - postoperative score) ÷ preoperative score] × 100%. " (NIR<25%), "effective" (25%≤NIR<60), "significantly improved" (NIR≥60%), and "cured " (NIR=100%). Early Neurological Deterioration (END) was defined as NIR < 0 within 7 days after surgery. delayed Neurological Deterioration (DND) was defined as a decrease in NIR by at least one grade after one year of follow-up, and maintained or even continued to deteriorate by the end of follow-up. Secondary outcomes were recurrence and the occurrence of adverse events (including surgical complications and END). Time to recurrence was calculated from the date of initial surgery to the date of DSA reconfirmation.
Table 1. Venous Hypertensive Myelopathy Scale (VHMS)
Results
01
Demographic and clinical characteristics
The 1-year and 5-year follow-up rates of this study were 83.1% (54/65) and 50.8% (33/65), respectively. The mean age of the patients was 57.4 years (SD, 11.4), with a male-to-female ratio of 8:1. Most patients presented slowly and insidiously with a median disease duration of 7.2 months. The shortest duration of disease was 1 week and the longest was 5 years. 51.6% (33/65) of the patients had been misdiagnosed with other diseases (e.g., myelitis) and treated accordingly. Twenty-three patients were treated with preoperative steroids, of whom 65.3% deteriorated and 13.0% experienced transient remission. Cerebrospinal fluid laboratory tests showed common protein elevations (71.4%, 5/7) and occasional increases in total cell counts. However, further immunological evidence was lacking.
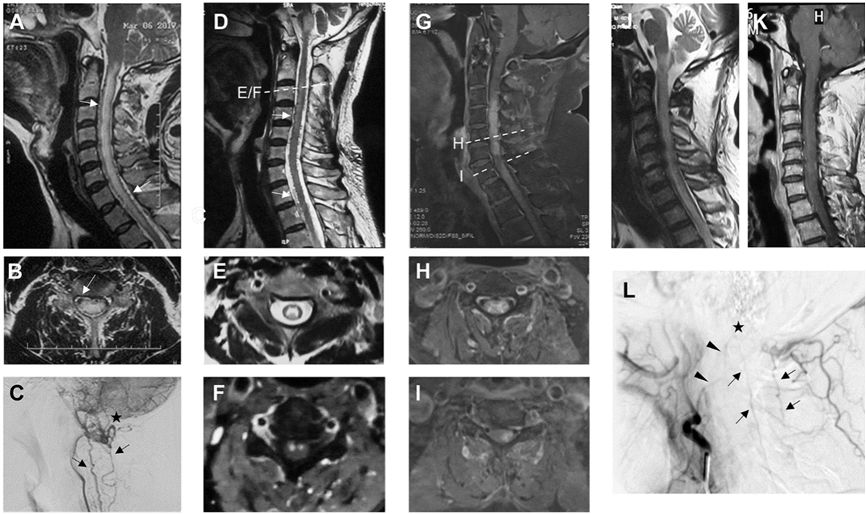
Figure 2. Representative imaging of CCJVHM patients
02
Clinical Presentation and Venous Hypertensive Myelopathy Scale
The clinical manifestations of CCJVHM are various neurological dysfunctions involving motor, sensory, urinary, defecation, and brainstem. Approximately half of the patients present with motor and sensory dysfunction at the initial onset of the disease, and this percentage rises to more than 90% by the time of admission (Figure 3A). Motor and sensory dysfunction was more common in the lower extremities compared to the upper extremities. In addition, 27.7% (18/65) of patients presented with paralysis of one limb. Notably, approximately one quarter (16/62) of patients complained of limb weakness or decreased motor endurance, but there was no evidence of decreased muscle strength on examination. In addition, patients' sensory planes were usually below the level of the lesion (56.9%, 25/44). Urinary and defecation disturbances were also progressive, increasing from 20% at presentation to 67.7% at admission. Brainstem involvement was the most unique and dangerous presentation of CCJVHM compared to thoracolumbar VHM. A total of 41.5% (27/65) of patients complained of disturbances in brainstem function and neurological clusters at the time of admission. Three patients presented with Wallenberg's syndrome. Five patients presented with respiratory distress, three of whom progressed to severe respiratory depression after steroid treatment.
Based on the above symptoms, JOA and ALS may not be fully applicable to the neurological function evaluation of CCJVHM. vHMS has a higher evaluation dimension compared to the above two scales (Figure 3B). The ROC curve to predict the occurrence of early postoperative neurological deterioration showed that the area under the curve of JOA and mALS was about 80% of that of VHMS (Figure 3C). Of course, the correlation between VHMS and JOA/ALS scores was relatively good (n=65, Figure 3D). Sensitivity analysis was performed by excluding patients who did not fit the JOA score. It was found that the linear fit between JOA and VHMS improved, with an increase in R² from 0.6722 to 0.7984 (n=14, Figure 3E). A sensitivity analysis of the linear relationship between ALS and VHMS was not performed because only one patient was suitable for the ALS score.
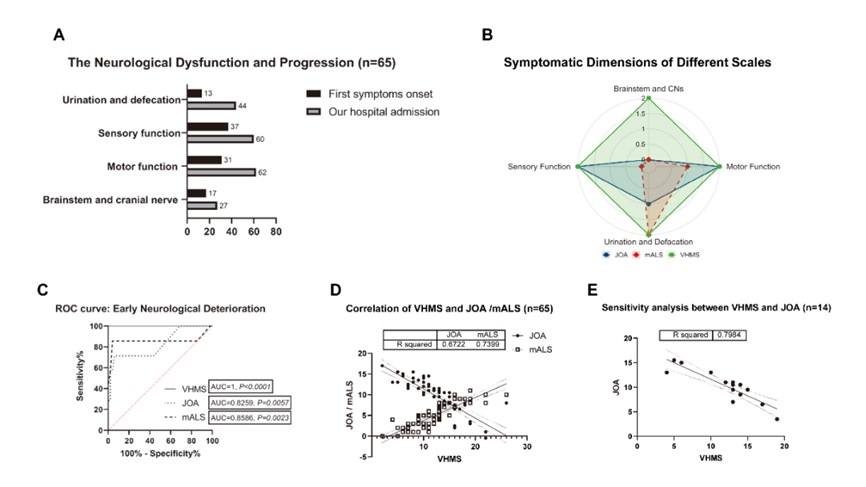
Figure 3. Comparison of clinical manifestations and different scales of CCJVHM
03
Long-term follow-up of neurological function after surgery
In this study, VHMS was used to analyze neurological functional outcomes. Two-thirds of the patients (23/33) showed dynamic changes in postoperative neurological function during the 5-year follow-up. The majority of patients improved effectively within the first year after surgery (Figure 4A, median NIR: 30.0%; IQR: 8.6%-56.9%, p=0.0075). 63.6% (21/33) of patients showed no significant improvement in neurological function within 7 days after surgery, including 5 cases with a sudden worsening of symptoms (Figure 4B). One patient developed a new respiratory rhythm abnormality after awakening from anesthesia, but recovered 1 month after mechanical ventilation. The proportion of patients who improved postoperatively (NIR ≥25%) peaked at the one-year follow-up (54.5%, 18/33), and one patient achieved a complete "cure". However, the proportion of patients with neurological decline tended to increase each year, with a five-year cumulative DND incidence of 24.2% (8/33). The chi-square trend test for decline in neurological function was not statistically significant, indicating a positive long-term outcome of surgical intervention in all patients (Figure 4B, p=0.3918).
Among patients who completed 1-year follow-up, 25.9% (14/54) developed DND and 13.0% (7/54) developed END. 3 of the patients who developed END improved at 1 year after follow-up, but 2 converted to DND. factors influencing DND were determined by multifactorial logistic regression. The results supported age as an independent predictor (Figure 4C; OR, 7.831; 95% CI, 1.090-56.266). For patients older than 65 years, the risk of DND increased approximately 8-fold. similar results were obtained from Kaplan-Meier analysis. Older patients had a higher risk of DND (Figure 4D; HR, 6.713; 95% CI, 1.724-26.14). The median time to DND in the elderly population was 7 years, and their progression-free rates at 3, 5, and 7 years were 76%, 61%, and 30%, respectively.
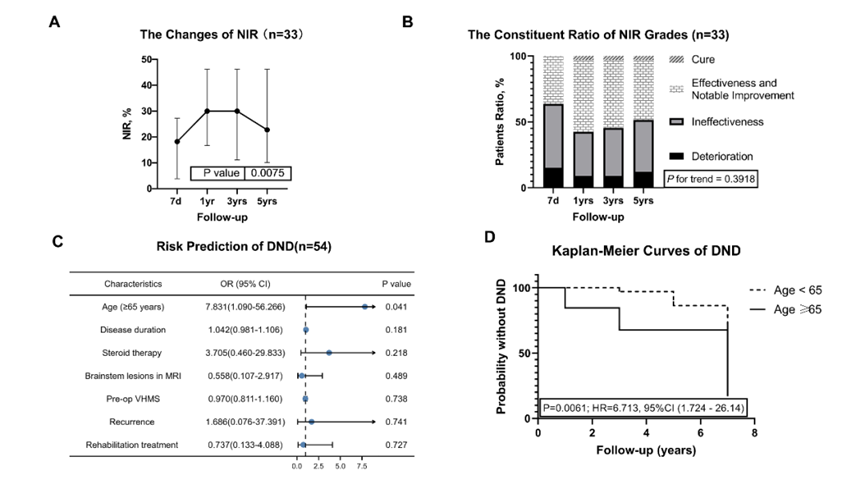
Figure 4. Postoperative neurological function analysis
04
Recurrence and postoperative adverse events
All nine recurrent patients (13.8%) had dural arteriovenous fistulas, corresponding to the two recurrence patterns shown in Figure 5. The first one was revascularization (Figure 5A-L). A total of eight patients underwent transarterial embolization at the time of first treatment. five patients used Onyx as embolic material, and three patients underwent reoperation for embolic recanalization. The recurrence rate was higher in the embolization group than in the surgical group (Table 3, p=0.007). Kaplan-Meier analysis showed an 11-fold increased risk of recurrence in the embolization group (median time to recurrence=34 months, p<0.0001, Figure 6A). Another pattern of recurrence was a de novo contralateral supplying arteriovenous fistula. Four patients (3 with surgery and 1 with embolization) had this type of recurrence, and their draining veins could be the same (Figure 5O/S, n=3) or different (Figure 5I/J, n=1) from the first disease. The remaining patients with recurrence (1 surgery, 2 embolization) could not be accurately determined the cause because of the lack of first imaging data. Most of the recurrent patients (8/9, 88.9%) underwent secondary treatment with microsurgery at our institution.
For the first treatment, the complication rate tended to be higher in the surgical group than in the endovascular treatment group, but the difference was not statistically significant (Table 3, p=0.5810). One patient died within 14 days after surgical treatment for a cause considered to be central respiratory failure causing severe pneumonia. Multifactorial logistic regression analysis showed that a history of recurrence increased the risk of postoperative adverse events (OR, 20.455; 95% CI, 1.170-357.320; p=0.039; Figure 6B). 55.6% (5/9) of patients with recurrence had an adverse event after the second treatment. four patients developed acute neurological deterioration, three of whom were treated for the first time with endovascular treatment. Intracranial infection occurred in two patients whose first treatment was surgical.
Table 3: Clinical classification and secondary outcomes of CCJVHM
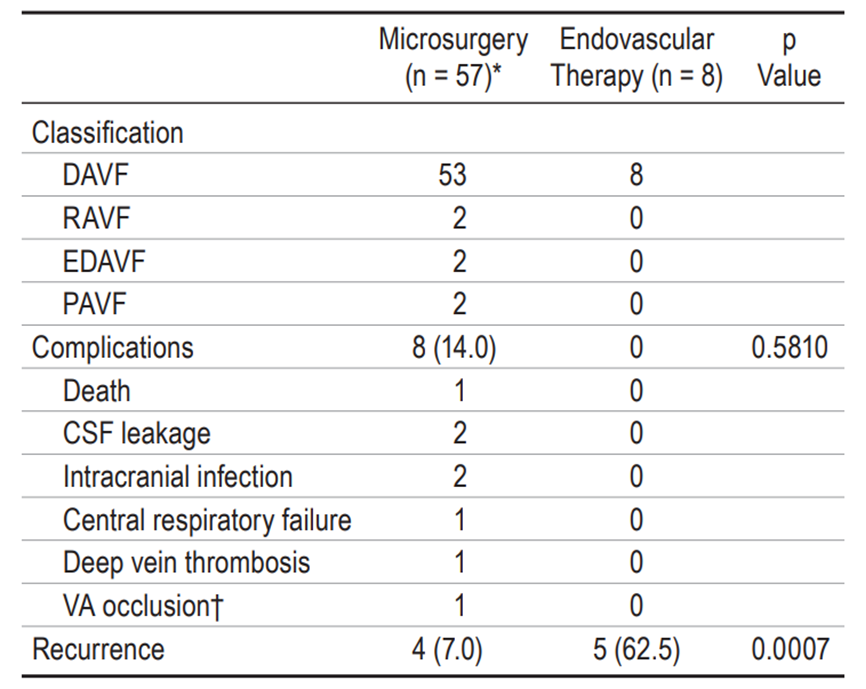
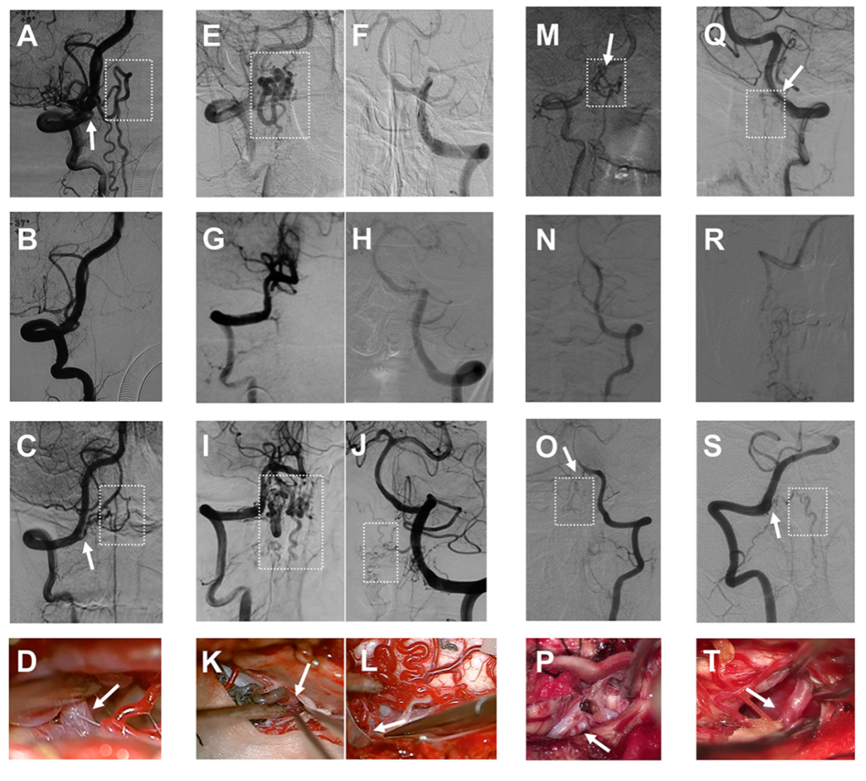
Figure 5. Angiographic and intraoperative images of recurrent patients
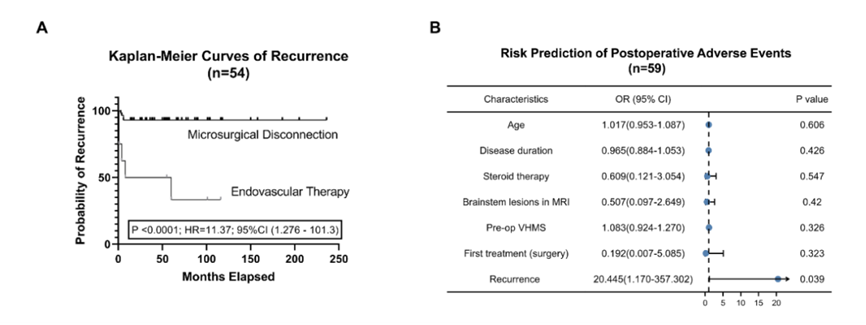
Figure 6. analysis of recurrence and adverse events
Conclusion
In summary, this study is an important update of the clinical features and long-term follow-up of venous hypertensive myelopathy. We summarize the unique clinical features of venous hypertensive myelopathy in the craniocervical junction region and propose a new venous hypertensive myelopathy rating scale. The primary outcome reveals that more than a quarter of patients present with delayed neurological deterioration. The risk of delayed neurological deterioration was increased eightfold in patients over 65 years of age at the time of first visit. Embolization recanalization is a cause of recurrence, but attention should also be paid to new fistulas of the contralateral blood supply. Moreover, the risk of postoperative complications is increased 20-fold with secondary treatment, regardless of the initial treatment plan. Therefore it is reasonable to aim for a one-time anatomical cure in experienced centers for this group of patients.
Corresponding Author
Prof. Dr. Zhang, Hongqi
Xuanwu Hospital, Capital Medical University, Department of Neurosurgery
Professor of Neurosurgery, Senior Consultant Neurosurgeon
Director of the Department of Neurosurgery, Xuanwu Hospital, Capital Medical University
For many years, Prof. Dr. Zhang, Hongqi has been engaged in the surgical and interventional treatment of cerebral and spinal cord vascular diseases, and his clinical and research work in cerebral aneurysm, craniocerebral vascular malformation and spinal cord vascular malformation is at the leading level at home and abroad. He has undertaken and completed 20 research projects at all levels, including the National Key Research and Development Project of the 13th Five-Year Plan and the National Natural Science Foundation of China, and has published more than 170 papers in JAMA Neurology, BRAIN, Annals of Neurology and other academic journals. Second Class Award.
Any use of this site constitutes your agreement to the Terms and Conditions and Privacy Policy linked below.
A single copy of these materials may be reprinted for noncommercial personal use only. "China-INI," "chinaini.org" are trademarks of China International Neuroscience Institute.
© 2008-2021 China International Neuroscience Institute (China-INI). All rights reserved.