doi: 10.1007/s10143-024-02743-z.
On August 29, 2024, the team of Professor Zhang Hongqi from the Department of Neurosurgery at Xuanwu Hospital of Capital Medical University published a research paper entitled “Microsurgical Treatment for Superior Petrosal Sinus Dural Arteriovenous Fistulas” in the journal Neurosurgical Review (JCR Q1, IF: 2.5). The co-first authors were Consultant Neurosurgeon Dr. Sun Liyong and post graduate student Su Xin from the Department of Neurosurgery at Xuanwu Hospital, and the corresponding author was Professor Zhang Hongqi from the Department of Neurosurgery at Xuanwu Hospital, Capital Medical University.
Keywords: superior petrosal sinus (SPS) dural arteriovenous fistula (DAVF), microsurgery, venous hypertensive spinal disease, intraparenchymal or subarachnoid hemorrhage
Abstract
Superior petrosal sinus (SPS) dural arteriovenous fistula (DAVF), also known as petrosal DAVF, is a common DAVF in the cavernous sinus region, most of which are associated with the drainage of the petrosal vein and its collateral branches, and occasionally require microsurgical intervention for treatment. This study attempts to elucidate the relationship between the drainage pattern and clinical manifestations by analyzing the drainage pattern of the petrosal vein tributaries in the surgical field. This retrospective study reviewed 34 consecutive patients who underwent microsurgical treatment for SPS DAVFs. The mean age of the cohort was 52.8 ± 11.8 years, and 85.3% (29/34) were male. The main symptoms included venous hypertensive myelopathy (VHM) (55.9%) and intraparenchymal or subarachnoid hemorrhage (23.5%). 94.1% of the lesions were completely cured by the standard retro sigmoid approach.
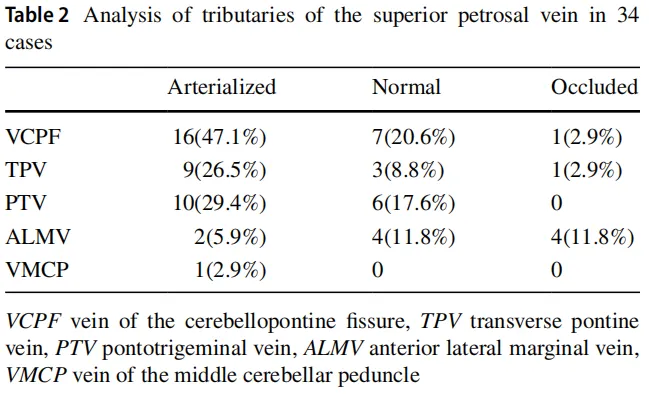
The most common arteriovenous branches of the internal carotid artery seen intraoperatively were the cerebellopontine fissure (VCPF), pons trigeminal vein (PTV), pons transverse vein (TPV), anterior lateral marginal vein (ALMV) and middle cerebellar peduncle vein (VMCP).
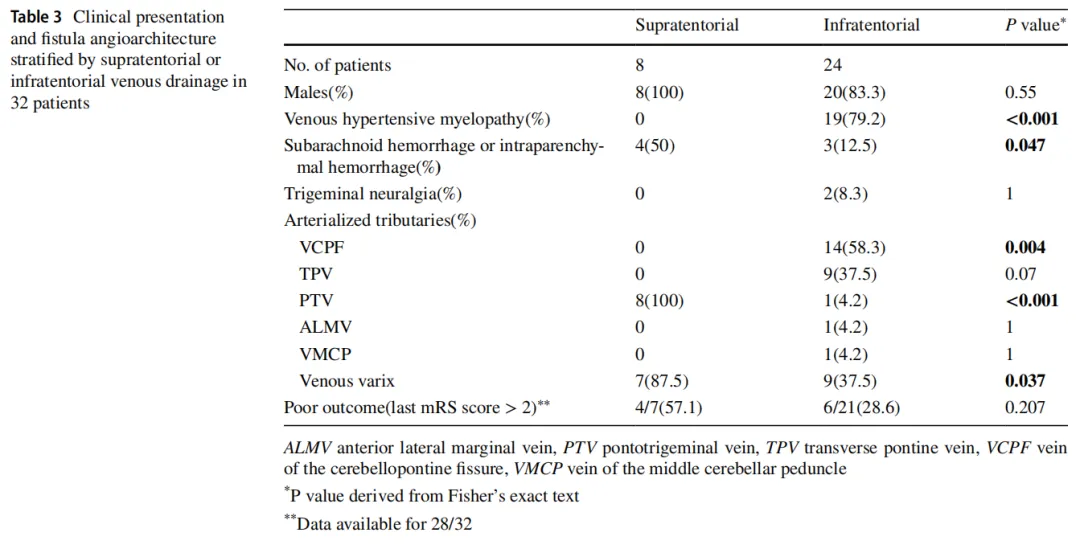
The supratentorial venous drainage pattern was associated with a higher incidence of intracranial hemorrhage and a higher proportion of venous malformations (P=0.047). Supratentorial venous drainage patterns were more frequently associated with the occurrence of VHM-related symptoms (P<0.001).
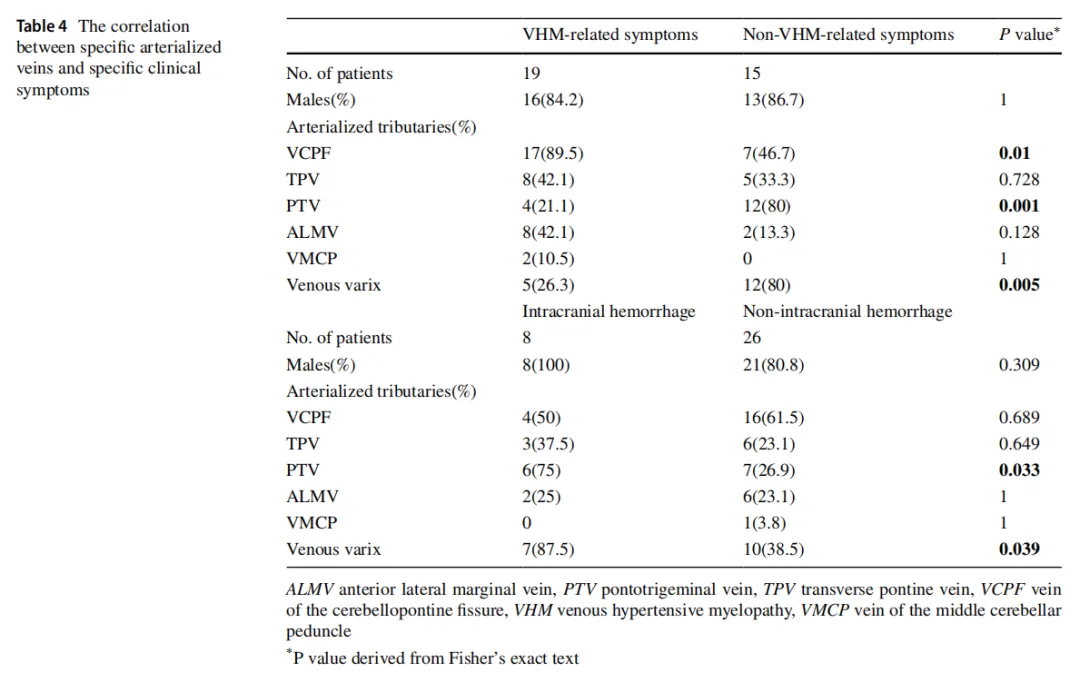
Patients with VHM-related symptoms showed a higher drainage proportion of the VCPF (P=0.01), while patients with intracranial hemorrhage symptoms showed a higher drainage proportion of the PTV (P=0.033).
Results
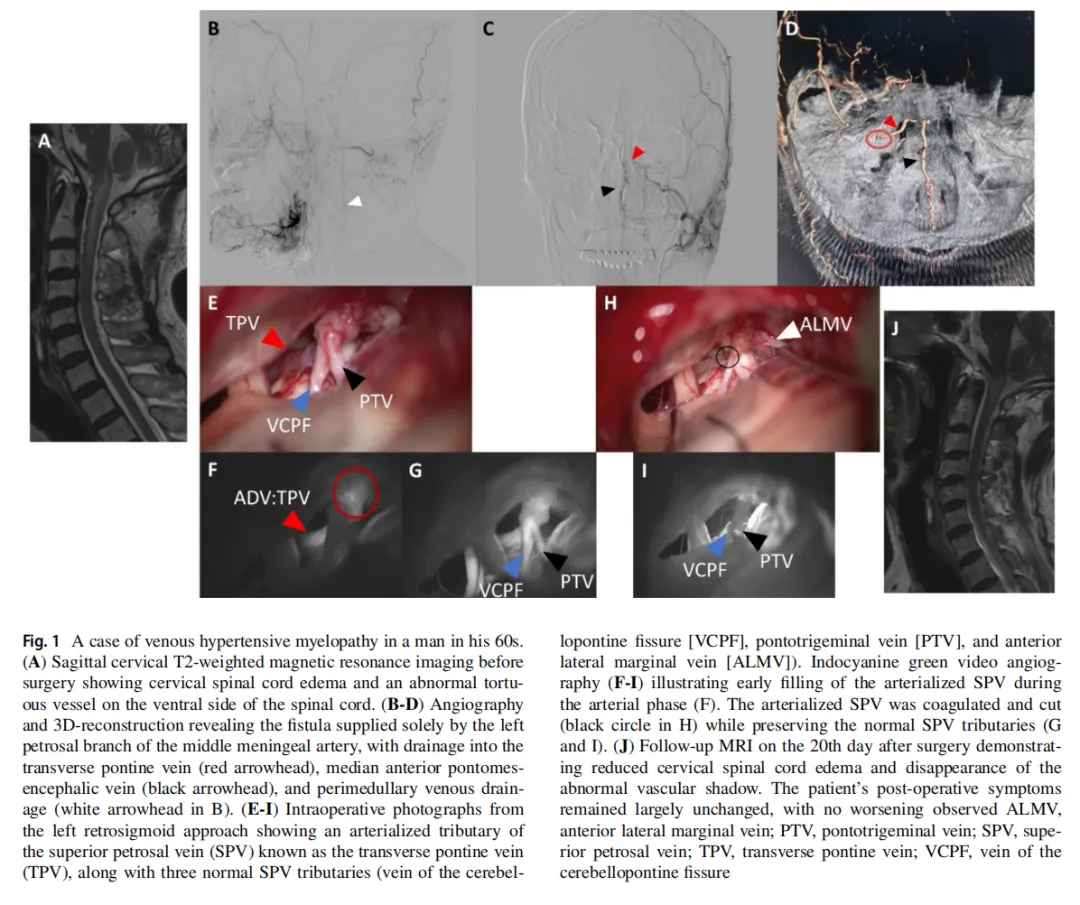
Figure 1. A case of venous hypertensive myelopathy in a man in his 60s(A)Sagittal cervical T2-weighted magnetic resonance imaging before surgery showing cervical spinal cord edema and an abnormal tortuous vessel on the ventral side of the spinal cord. (B-D) Angiography 3D-reconstruction revealing the fistula supplied solely by the left petrosal branch of the middle meningeal artery, with drainage into the transverse pontine vein (red arrowhead), median anterior Ponto mesencephalic vein (black arrowhead). and perimedullary venous drainage (white arrowhead in B).(E-l) Intraoperative photographs from the left retro sigmoid approach showing an arterialized tributary of the superior petrosal vein (SPV) known as the transverse pontine vein(TPV), along with three normal SPV tributaries (vein of the cerebellopontine fissure [VCPFl, Ponto trigeminal vein [PTV]. and anterior lateral marginal vein [ALMV]). Indocyanine green video angiography (F-D) illustrating early filling of the arterialized SPV during the arterial phase (F). The arterialized SpV was coagulated and cut(black circle in H) while preserving the normal SPy tributaries (Gand ). (J) Follow-up MRl on the 20th day after surgery demonstrating reduced cervical spinal cord edema and disappearance of the abnormal vascular shadow, The patient's post-operative symptoms remained largely unchanged.
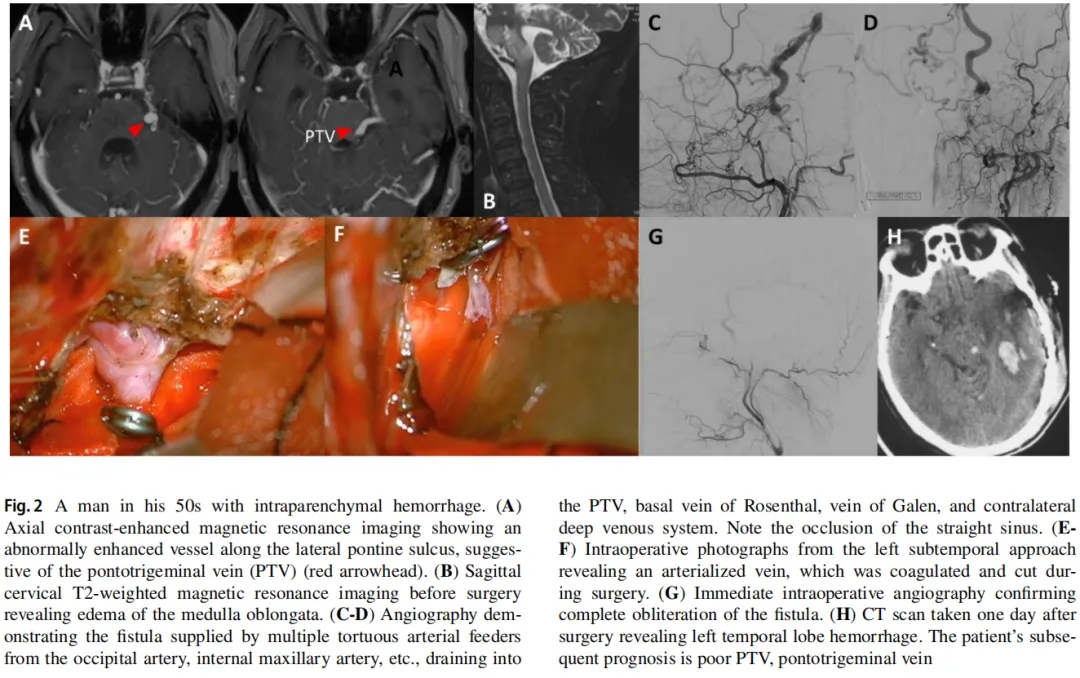
Figure 2. A man in his 50s with intraparenchymal hemorrhage. (A)Axial contrast-enhanced magnetic resonance imaging showing an abnormally enhanced vessel along the lateral pontine sulcus, suggestive of the Ponto trigeminal vein (PTV) (red arrowhead). (B) Sagittal cervical T2-weighted magnetic resonance imaging before surgery revealing edema of the medulla oblongata.(C.D) Angiography demonstrating the fistula supplied by multiple tortuous arterial feeder Strom the occipital artery, internal maxillary artery, etc.. draining into the PTV, basal vein of Rosenthal, vein of Galen, and contralateral deep venous system, Note the occlusion of the straight sinus. (E.F) Intraoperative photographs from the left sub temporal approach revealing an arterialized vein, which was coagulated and cut during surgery,(G)immediate intraoperative angiography confirming complete obliteration of the fistula. (H) CT scan taken one day after surgery revealing left temporal lobe hemorrhage, The patient's subsequent prognosis is poor PTV, Ponto trigeminal vein The patient's postoperative prognosis is poor.
Supplementary Information The online version contains supplementary material available at https://doi.org/10.1007/s10143-024-02743-z.(Video of the operation on a patient)
Conclusions
Interventional treatment of SPS DAVFs is sometimes risky and has limitations (presence of a proximal venous aneurysm in the draining vein; risk of facial paralysis, etc.). The correct identification of arterialized cavernous vein saphenous branches and the preservation of normal tributaries may prevent complications of venous infarction in the posterior cranial fossa. Surgical treatment via the standard retro sigmoid approach has good clinical results and a high cure rate, while the inferior temporal approach is not sufficient for exposing the draining veins. In cases of suboccipital venous drainage, the arteriovenous malformation tributary is most commonly the VCPF, which is usually associated with VHM-related symptoms. In cases of supratentorial venous drainage, the main arteriovenous malformation tributary is the PTV, which is usually associated with intracranial hemorrhage symptoms.

Co-first author
Sun Liyong
Capital Medical University Xuanwu Hospital
Department of Neurosurgery Consultant Neurosurgeon Lecturer
He graduated from Capital Medical University. He is a standing committee member of the Beijing Medical Association's Neurointerventional Branch and a member of the China Association for Science and Technology in Human Health's Clinical Neurotechnology Professional Committee.
He specializes in surgical and endovascular treatments for cerebrovascular diseases of the brain and spinal cord, such as cerebral aneurysms, cerebral vascular malformations, Moyamoya disease, dural arteriovenous fistulas, cavernous angiomas, spinal vascular malformations, and dural arteriovenous fistulas.
Clinic hours
Tuesday afternoon and Thursday (specialist clinic)

Co-first author
Su Xin
Xuanwu Hospital of Capital Medical University
2022-post graduate student of Surgery (Neurosurgery)
He majors in research on dural arteriovenous fistula, chronic subdural hematoma, dural arteriovenous fistula and other intracranial vascular malformations. He has Published more than 20 papers as the first and co-first author in SCI journals, 1 paper in a Chinese core journal, and participated in the translation of 2 books. Accepted 3 patents.

Corresponding author
Zhang Hongqi
Xuanwu Hospital Capital Medical University
Senior Consultant Neurosurgeon
Professor Doctoral Supervisor
He currently serves as the Director of the Neurosurgery Department at Capital Medical University Xuanwu Hospital. He is Currently an Executive Member of the World Federation of Interventional Neuroradiology (WFITN), an Executive Member of the Asian and Oceanian Federation of Interventional Neuroradiology (AAFITN), Chairman of the Neurointerventional Committee of the Chinese Medical Doctor Association, Member of the Standing Committee of the Neurosurgery Branch of the Chinese Medical Association, Executive Director of the Cardiovascular and Cerebrovascular Disease Committee of the Chinese Gerontology Society, Vice Chairman of the Neurosurgery Branch of the Beijing Medical Association Deputy Chairman, Editorial Board Member of the Chinese Journal of Cerebrovascular Diseases and Chinese Journal of Minimally Invasive Neurosurgery, Chief Editor of the Chinese version of JNIS. For many years, he has been engaged in the surgical and interventional treatment of brain and spinal cord vascular diseases, and his clinical and research work in cerebral aneurysms, cranial cerebrovascular malformations, and spinal cord vascular malformations is at the leading domestic and international level. He has undertaken and completed 20 research projects at all levels, including the National Key Research and Development Program during the 13th Five-Year Plan and projects funded by the National Natural Science Foundation of China. He has published more than 170 papers in academic journals such as JAMA Neurology, BRAIN and Annals of Neurology, and has won the second prize of the National Science and Technology Progress Award.
Clinic hours
Tuesday evenings (special clinic)
Any use of this site constitutes your agreement to the Terms and Conditions and Privacy Policy linked below.
A single copy of these materials may be reprinted for noncommercial personal use only. "China-INI," "chinaini.org" are trademarks of China International Neuroscience Institute.
© 2008-2021 China International Neuroscience Institute (China-INI). All rights reserved.