Keywords
Acute ischemic stroke Coagulation-fibrinolysis-endothelial system New thrombosis four items
One minute to understand the article
What are the new thrombosis four items?
The thrombosis process mainly involves three major systems: vascular endothelium, coagulation and fibrinolysis. It has been confirmed that when the body is in a prothrombotic state, these three major systems have begun to change. At present, the routine coagulation four-item test in clinical laboratories is not very sensitive to hypercoagulable states. Although D-dimer and fibrin (pro)degradation products (FDP) are widely used as markers of hypercoagulable states and hyperfibrinolysis, they are produced after thrombosis, and are therefore passive, late detection items that are not sensitive in predicting the pre-thrombotic state.
The new thrombosis four items include thrombin-antithrombin complex (TAT), plasmin-α2 plasmin inhibitor complex (PIC), tissue plasminogen activator-plasminogen activator inhibitor complex (t-PAIC) and soluble thrombomodulin (sTM). They are elevated to varying degrees when hypercoagulation, fibrinolysis or vascular endothelial damage occurs, and are effective indicators of early changes in the body's vascular endothelium, coagulation and fibrinolysis systems. Among them, TAT and PIC are markers for the initiation of the coagulation and fibrinolysis systems, respectively. t-PAIC can reflect the degree of vascular endothelial damage and the inhibitory state of the fibrinolysis system, while sTM is a marker of vascular endothelial damage. Therefore, the new thrombosis four items are gradually being used for thrombus risk screening, early diagnosis, disease assessment, and another efficacy evaluation such as thrombolysis.
Abstract
Objective
This study aimed to explore the characteristics of changes in the content of the new thrombosis four items in the proximal blood (ischemic local) and peripheral femoral artery blood of patients with acute large vessel occlusion stroke (AIS-LVO) treated with endovascular thrombectomy (EVT), and its relationship with patient clinical characteristics, prognosis, and surgical parameters.
Methods
A prospectively maintained clinical database and biorepository (arterial blood from the ischemic microenvironment—proximal blood; femoral artery blood—peripheral self-control) were used to retrospectively include 166 AIS-LVO patients (mean age 62±11.54 years; 34.3% female).
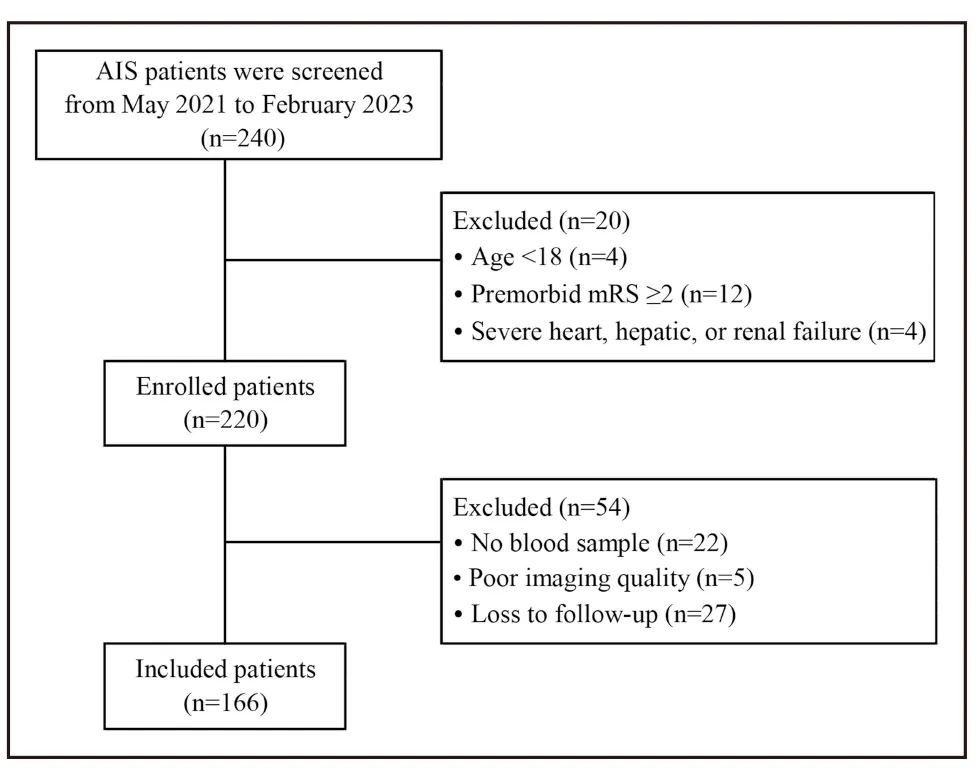
Figure 1: Patient selection flowchart
Results
We first found that compared to systemic levels, TAT, PIC, t-PAIC and D-dimer levels were significantly elevated in the ischemic region, while sTM levels were significantly reduced (Figure 2A). Subsequently, we analyzed the effect of rt-PA thrombolysis on these thrombotic and hemostatic molecules. We found that the peripheral and ischemic region t-PAIC and D-dimer levels of AIS-LVO patients who received IVT before EVT (n=23, 13.9%) were significantly higher than those of patients who did not receive IVT. However, there was no significant difference in TAT, PIC and sTM levels between the two groups. These results indicate that rt-PA treatment induces a higher state of fibrinolysis (Figure 2B). Finally, we analyzed the differences in thrombotic and hemostatic molecules between different stroke etiologies and found that the levels of TAT and PIC in the ischemic region of patients with cardioembolic stroke were significantly higher than those in patients with large atherosclerotic stroke. However, there were no significant differences in the levels of thrombotic and hemostatic molecules between the cardioembolic stroke group and the cryptogenic stroke group, or between the large atherosclerotic stroke group and the cryptogenic stroke group (Figure 2C).
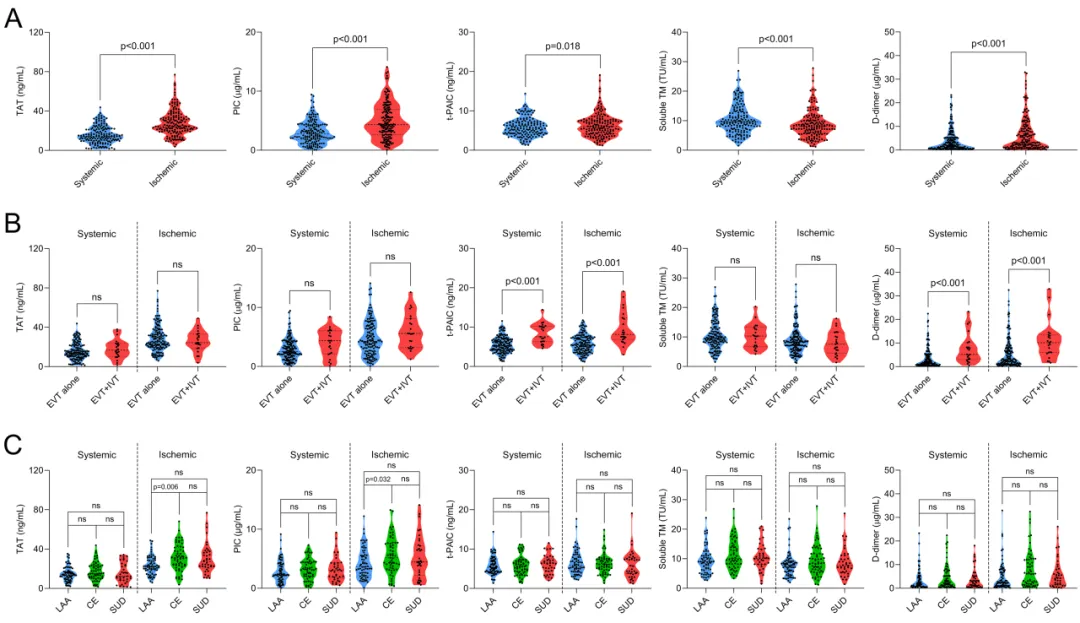
Figure 2: Levels of thrombotic and hemostatic molecular markers in the hyperacute phase of AIS-LVO
We then performed a series of correlation analyses and found that some thrombotic and hemostatic molecular levels in the periphery and ischemic region were correlated with clinical characteristics, prognosis, and surgical parameters of patients (Figure 3).
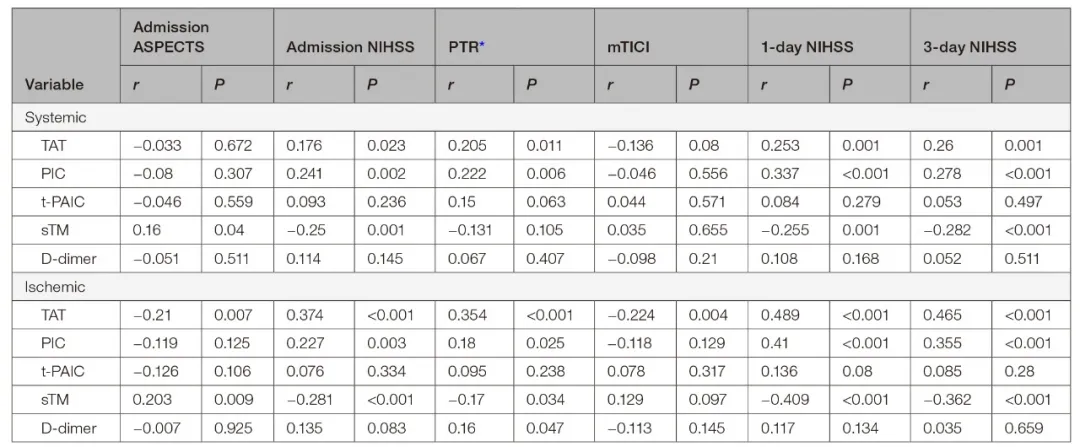
Figure 3: Correlation analysis of thrombotic and hemostatic molecules with clinical characteristics, prognosis, and surgical parameters of patients
Finally, we found that the levels of TAT and PIC in the ischemic region were significantly associated with the risk of symptomatic intracranial hemorrhage, and the levels of TAT and PIC in the ischemic region and sTM were significantly associated with an increased risk of poor prognosis (mRS score 3-6) at 90 days. These thrombotic and hemostatic molecules, whether analyzed individually or in combination, significantly enhanced the predictive power of traditional risk factors for prognosis (Figure 4).
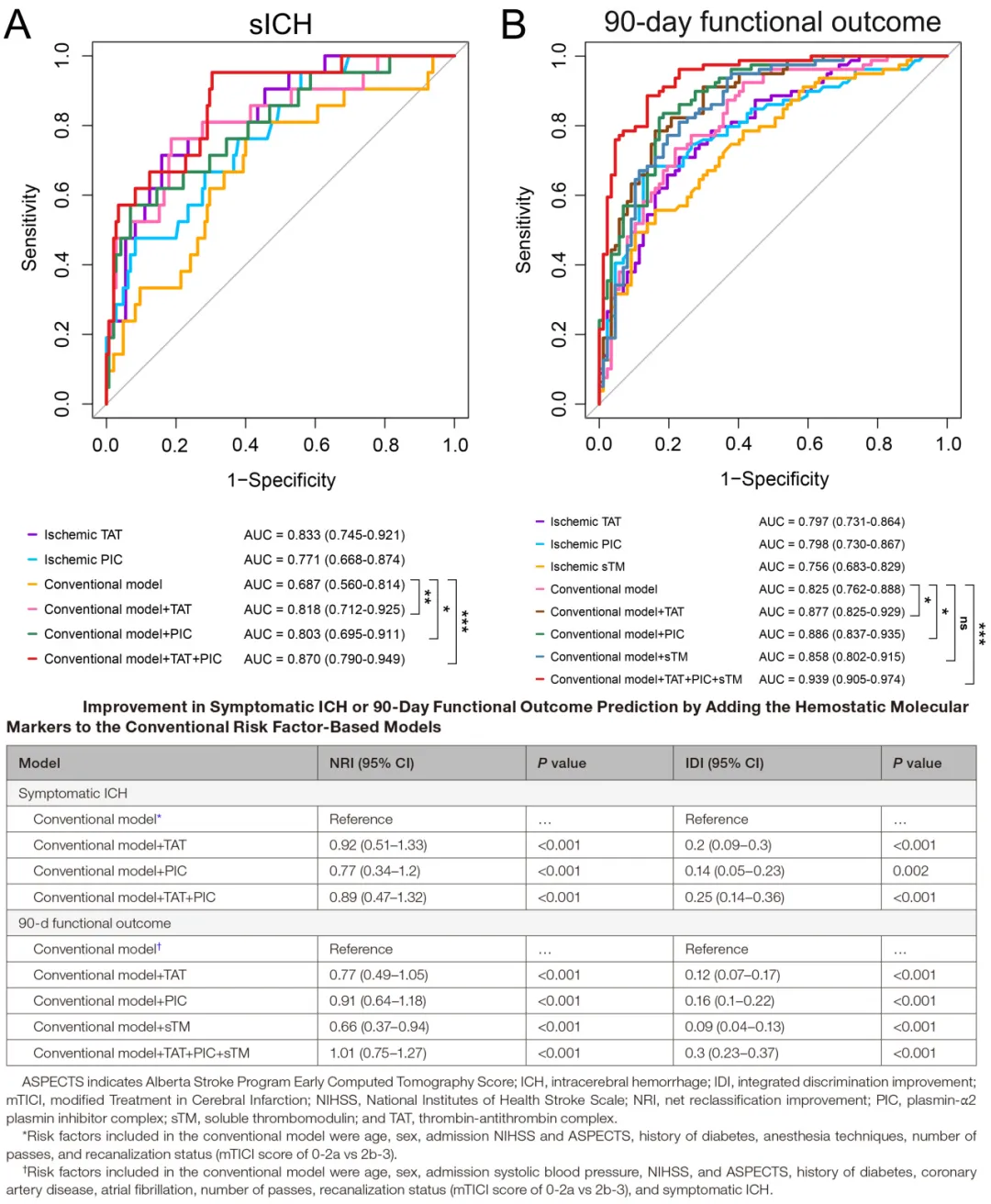
Figure 4: Relationship between thrombotic and hemostatic molecules and symptomatic intracranial hemorrhage and adverse 90-day outcomes
Conclusion
We observed that the coagulation-fibrinolytic system was in a state of hyperactivation in localized ischemic regions during the hyperacute phase in patients with AIS-LVO. Rapid detection of these thrombotic and hemostatic molecular markers, especially TAT, PIC and sTM, during interventional therapy may provide valuable information for stroke risk stratification and therapeutic decision-making and therefore deserves further research.

First Author/Corresponding Author
Xu Xin
Xuanwu Hospital, Capital Medical University
Resident Neurosurgeon of the Department of Neurosurgery, associate research fellow
He is a Neurosurgeon and Associate Researcher at Xuanwu Hospital of Capital Medical University, PhD jointly trained by Tianjin Medical University/University of Washington. He is mainly engaged in basic and clinical translational research on ischemic cerebrovascular disease and traumatic brain injury. He is currently in charge of one general and one youth project of the National Natural Science Foundation of China, and has been selected for talent programs such as the Beijing Medical Management Center's “Young Talent” program and the Taishan Scholar Young Expert Program. In recent years, he has published 15 SCI papers as the first/co-first/corresponding author in internationally renowned journals such as Blood, J Neurosurg, J Thromb Haemost, J Neuroinflamm, and JAHA, with a cumulative impact factor of over 150 points.

Corresponding author
Jiao Liqun
Vice President of Xuanwu Hospital, Capital Medical University
Senior Consultant Neurosurgeon, Professor, Doctoral Supervisor
He is the Vice President of Xuanwu Hospital, Capital Medical University, Director of the Interventional Radiology Department, Deputy Director of the Department of Neurosurgery, Director of the Cerebral Blood Flow Reconstruction Center, and President of the National Regional Medical Center and Xuanwu Hospital Jinan Hospital. He is also the editor-in-chief of the Chinese Journal of Cerebrovascular Diseases, deputy chairman of the Neurointerventional Committee of the Chinese Medical Doctor Association, chairman of the Neurointerventional Committee of the National Health Commission Continuing Education Center, chairman of the National Health Commission Brain Prevention Committee Ischemic Stroke Surgery Committee, deputy chairman of the National Health Commission Brain Prevention Committee Ischemic Stroke Intervention Committee, and vice president of the Beijing Interventional Medicine Association. He graduated from Shandong Medical University and successively studied under Professor Zhu Shugan and Professor Ling Feng, obtaining a master's degree and a doctorate in neurosurgery. He also completed postdoctoral research at Peking University under the guidance of Professor Bao Shengde. He specializes in the surgical and interventional treatment of ischemic cerebrovascular disease, and was the first in the world to carry out innovative surgeries such as combined surgery for the treatment of carotid artery occlusion and vertebral artery occlusion, as well as drug-coated balloon treatment for vertebral artery stenosis. He has also led the Cerebrovascular Reconstruction Center of Xuanwu Hospital in in-depth research in this field, and has also long emphasized education and training, training a large number of highly qualified doctors in China.
Any use of this site constitutes your agreement to the Terms and Conditions and Privacy Policy linked below.
A single copy of these materials may be reprinted for noncommercial personal use only. "China-INI," "chinaini.org" are trademarks of China International Neuroscience Institute.
© 2008-2021 China International Neuroscience Institute (China-INI). All rights reserved.