Li T, Yang R, Wang J, Wang T, Liu G, Jin J, Bai X, Xu R, Lu T, Wang Y, Dmytriw AA, Yang B, Jiao L. Anatomical predispositions for silent cerebral infarction post carotid artery stenting: A retrospective cohort. Int J Surg. 2024 Jun 19. doi: 10.1097/JS9.0000000000001833. Epub ahead of print. PMID: 38896855.
Keywords: asymptomatic cerebral infarction, carotid artery stenting, anatomical features, nomogram
One-minute summary:
Ischemic cerebrovascular events caused by carotid artery stenosis impose a significant and heavy burden on the health status of individual patients and the socioeconomic system. In view of the rapid development of interventional medical technology, carotid artery stenting (CAS) has become an important alternative treatment for carotid endarterectomy, and its clinical status is becoming increasingly prominent. Currently, silent cerebral infarction (SCI) after CAS has become a widely focused issue in the medical community due to its high incidence (between 18% and 57%) and its subsequent possible increased risk of long-term cognitive decline, dementia, and future cerebrovascular events. In this context, reducing the incidence of SCI after CAS has become a key scientific issue that needs to be urgently addressed. The importance of anatomical features as key factors affecting the efficacy of CAS surgery and the risk of complications is self-evident. Previous studies have shown that certain anatomical variations, such as type III aortic arch morphology and a higher proximal tortuosity index, are potentially associated with an increased risk of SCI after CAS, but the specific mechanism remains to be further elucidated. In addition, the relationship between factors such as the specific morphology of the aortic arch, relevant anatomical parameters of the common carotid artery, and other factors and SCI is still in the preliminary exploratory stage, and a comprehensive and in-depth analysis is lacking. More critically, no study has been able to systematically integrate multiple anatomical factors to construct a customized tool or model that can effectively predict the risk of SCI after CAS.
In view of this, this present study aims to deeply analyze the potential anatomical risk factors for the occurrence of SCI after CAS, and innovatively construct a prediction model based on a nomogram through the comprehensive application of statistical and clinical imaging techniques. The model aims to provide more accurate and personalized treatment strategies and plan suggestions based on the individual anatomical characteristics of patients, with a view to improving the safety of CAS treatment while further optimizing its therapeutic effect and bringing more significant health benefits to patients.
Background
Silent cerebral infarction (SCI) after carotid artery stenting (CAS) is believed to be associated with cognitive decline, the development of dementia, and an increased risk of subsequent cerebrovascular events.
This study aimed to explore the potential anatomical factors associated with the occurrence of SCI after carotid artery stenting and further develop a predictive nomogram to accurately predict the risk of SCI after CAS.
Methods
This study retrospectively reviewed the data set of 250 patients with carotid artery stenosis who underwent CAS at Xuanwu Hospital between June 2020 and November 2021.
Stratified by the date of surgery, the participants were assigned to the training cohort and the validation cohort.
Multivariate logistic regression analysis was used to identify prognostic risk factors and construct nomograms.
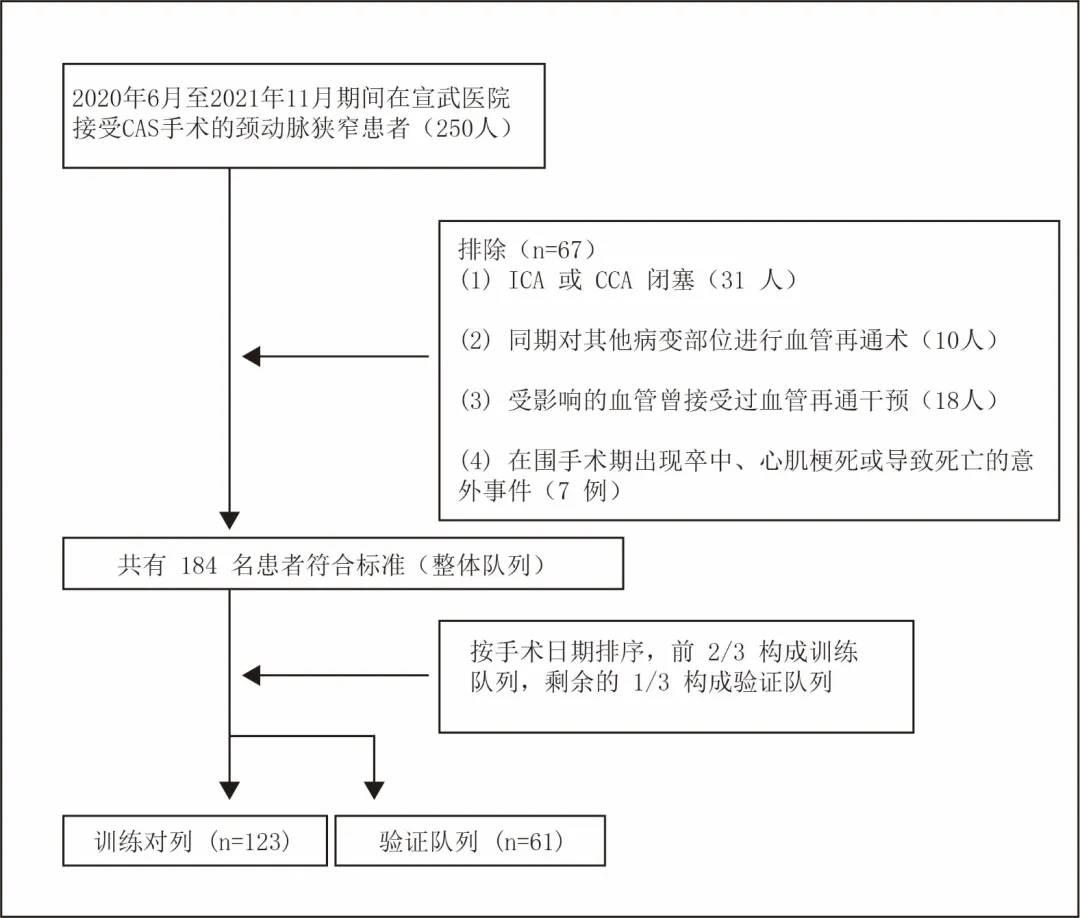
Figure 1: Flow chart of the screening process Results
Results
A total of 184 patients were included in the study, of whom 60 (32.6%) had SCI and 124 (67.4%) did not. In the training cohort (n=123), age (OR 1.08, 95%CI 1.01-1.16; P=0.034), aortic arch type (type III vs. type I: OR 10.79, 95%CI 2.12-54 .81; P=0.005), aortic arch variants (OR 47.71, 95%CI 6.05-376.09; P<0.001), common carotid artery (CCA) opening lesions (OR 6.93, 95%CI 1.49-32.32; P=0.014) and proximal tortuosity index (TI) (OR 1.01, 95%CI 1.00-1.02; P=0.029) were identified as independent risk factors for SCI after CAS. The nomogram had a concordance index (C-index) of 0.89 (95% CI, 0.84–0.95) in the training cohort. Furthermore, the nomogram demonstrated commendable validity in the validation cohort (C-index=0.94) and in the entire participant population (C-index=0.90). Also, decision curve analysis indicated that the nomogram was exemplary for clinical application.
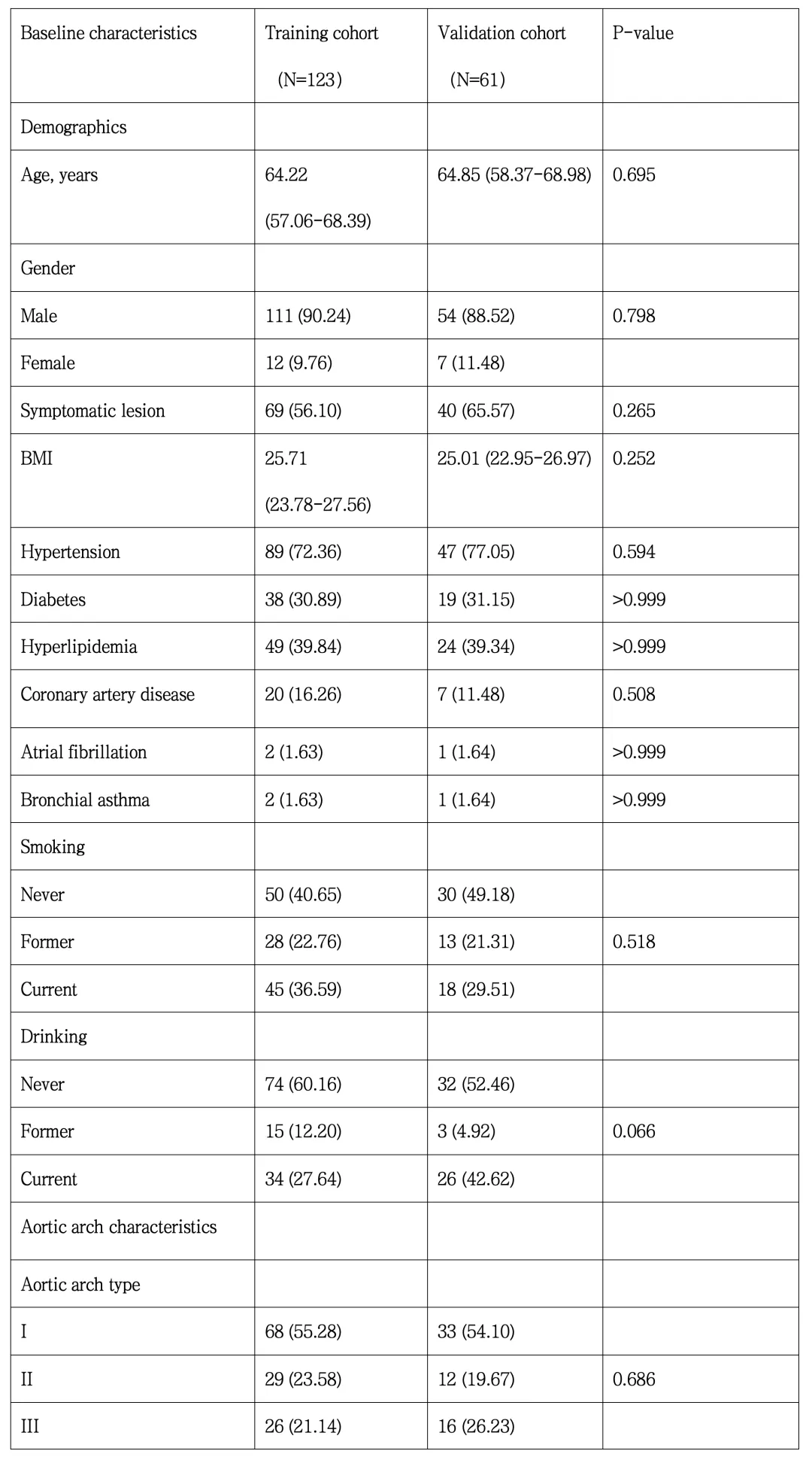
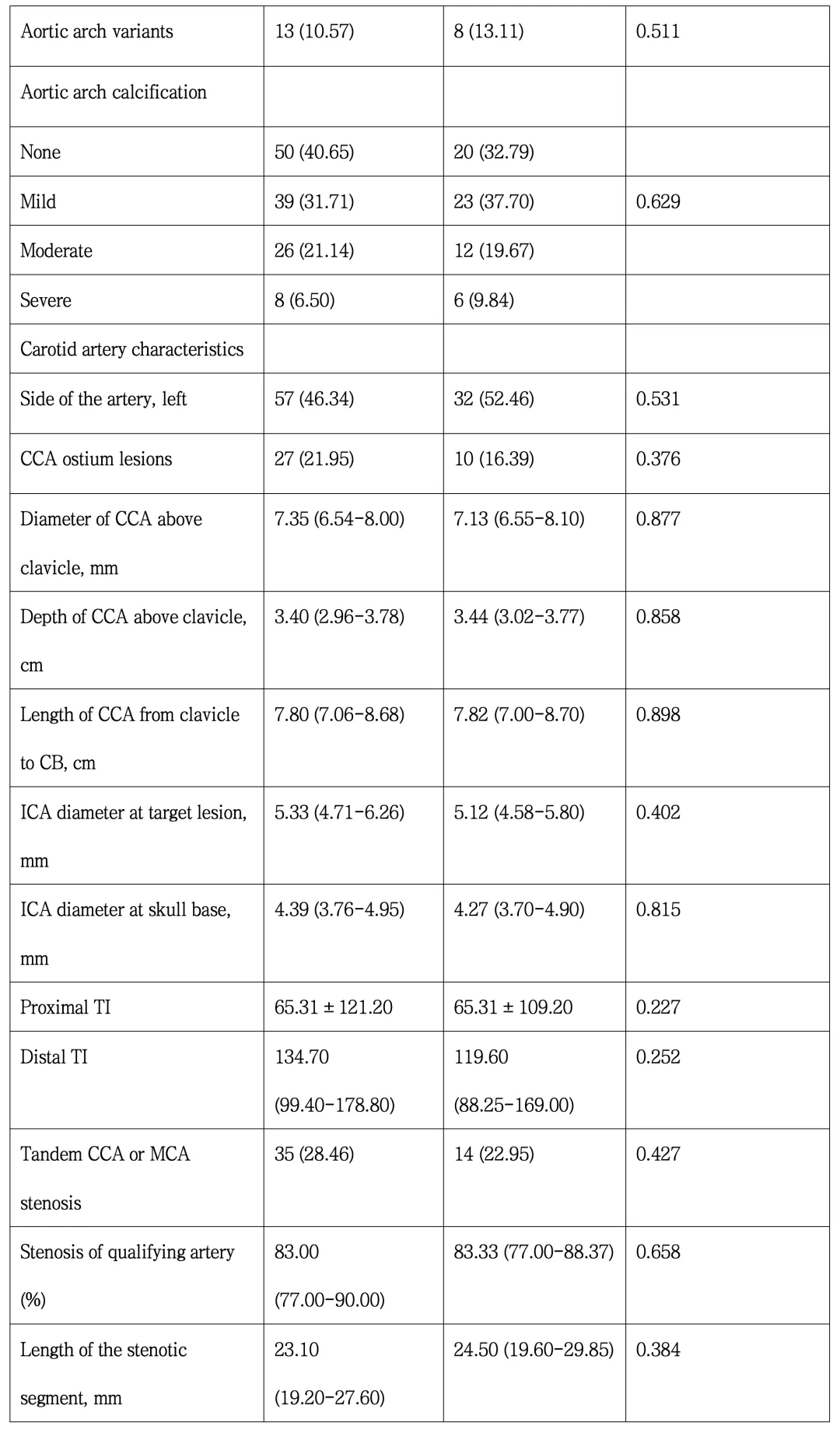
Table 1. Demographic and anatomical characteristics of the training and validation cohorts 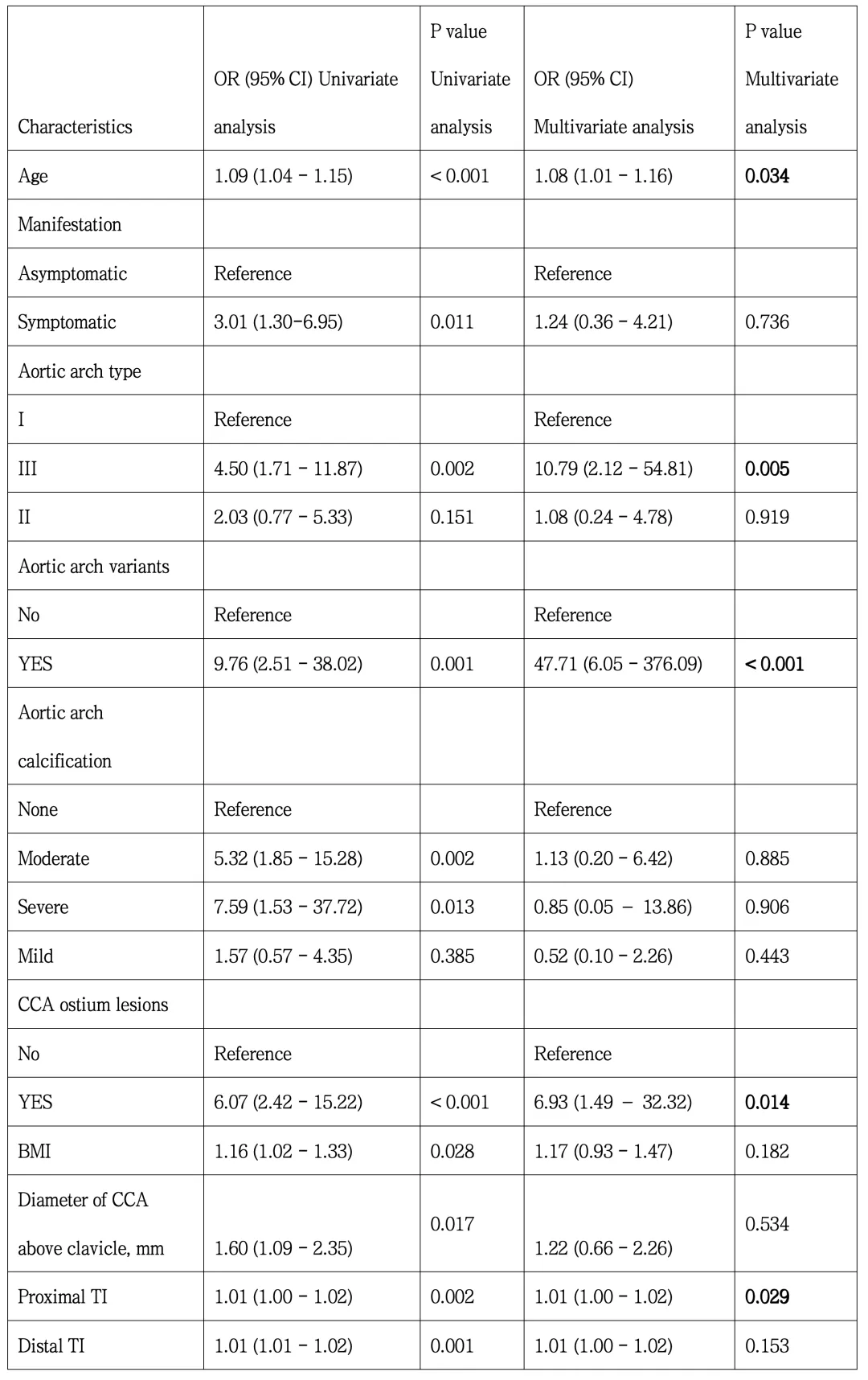
Table 2. Results of the logistic regression analysis of the training cohort

Figure 2. Nomogram for predicting the likelihood of SCI after CAS and its validation and assessment
(A) Nomogram based on the results of the multivariate logistic analysis of the training cohort. (B) Decision curve analysis of the nomogram in the training cohort. (C-D) ROC trace results of the nomogram in the training and validation cohorts. (E-F) Calibration plots of the nomograms in the training and validation cohorts.
Conclusion
The results of this study showed that age, aortic arch type, aortic arch variation, CCA opening lesions and proximal TI are independent risk factors associated with SCI after CAS. The nomograms developed based on these risk factors have strong prognostic significance and can be used as an important auxiliary tool for clinical decision-making.
Professor Yang Bin's comments:
This study is a model of the team's exploration in the field of in-depth mining of retrospective databases. Its uniqueness lies in the fact that even though a seemingly traditional research structure was adopted – a single-center retrospective database design, the standard method of multiple factor correlation analysis, and a focus on the conventional research subjects, namely carotid artery stenting (CAS) patients and their imaging characteristics, it successfully revealed age, aortic arch type, aortic arch anatomical variation, lesions at the opening of the common carotid artery, and proximal tortuosity index as independent predictors of stroke complications (asymptomatic cerebral infarction, SCI) after CAS. Furthermore, the nomogram constructed based on these key risk factors shows significant value in prognostic assessment and provides a strong quantitative support tool for clinical decision-making. In contrast to the traditional retrospective data mining approach, the research team followed a more rigorous and goal-oriented research paradigm: First, through in-depth integration of clinical practice experience and detailed literature research, the core scientific problem to be solved was accurately refined; then, a retrospective database that fits well with this core problem was carefully constructed to ensure that the database design directly serves the answer to the scientific question. This innovative research approach not only improves the efficiency and pertinence of data mining, but also lays a solid scientific foundation for subsequent improvement of clinical practice and formulation of personalized treatment strategies.
Co-first author
Li Tianhua
Xuanwu Hospital Capital Medical University
Department of Neurosurgery Doctoral student

He is a doctoral student in the Department of Neurosurgery at Xuanwu Hospital, Capital Medical University, under the supervision of Professor Jiao Liqun.
Research interests:
Basic and clinical research on ischemic cerebrovascular disease.
Scientific research experience:
He has participated in the Beijing Municipal Administration of Hospitals' municipal hospital clinical medicine development project (the “Sailing” program), the Beijing Natural Science Foundation (youth project), and 3 research projects of the Xuanwu Hospital National Natural Science Foundation.
So far, he has published 8 articles as the first or co-first author in SCI journals such as the International Journal of Surgery, Journal of Neurointerventional Surgery, European journal of neurology, and CNS Neuroscience & Therapeutics, and 1 article in a Chinese core journal.
Co-first author
Yang Renjie
Xuanwu Hospital Capital Medical University
Department of Neurosurgery Doctoral student

He is a doctoral student in the Department of Neurosurgery at Xuanwu Hospital, Capital Medical University, under the supervision of Professor Jiao Liqun. His main research direction is the surgical and interventional treatment of ischemic cerebrovascular disease and has published 3 SCI articles in JNIS, EJVES and other journals.
Co-first author
Wang Jie
Xuanwu Hospital Capital Medical University
Department of Neurosurgery Doctoral student

She is a doctoral student in the Department of Neurosurgery at Xuanwu Hospital, Capital Medical University, under the supervision of Professor Jiao Liqun.
Research direction:
Clinical research related to cerebral vascular stenosis.
Scientific research experience:
Currently, she has published 5 SCI papers as the first author or co-first author.
Corresponding author
Yang Bin
Department of Neurosurgery, Xuanwu Hospital, Capital Medical University, Consultant Neurosurgeon
He is a Doctor of Medicine. From November 2016 to June 2019, he studied under the famous neurosurgery expert Professor Ling Feng as a postdoctoral researcher, and is currently working in the Department of Neurosurgery of Xuanwu Hospital, Capital Medical University. His clinical expertise lies in the surgical and interventional treatment of ischemic cerebrovascular disease, and he is skilled in performing intracranial and extracranial arterial stenosis stenting, mechanical thrombectomy for acute ischemic stroke, and carotid endarterectomy. He has participated in six national and provincial research projects and published more than 10 papers, including seven SCI-indexed papers.
Corresponding author
Jiao Liqun
Vice President of Xuanwu Hospital, Capital Medical University
Senior Consultant Neurosurgeon Professor, Doctoral Supervisor

He is the Vice President of Xuanwu Hospital, Capital Medical University, Director of the Department of Interventional Radiology, Deputy Director of the Department of Neurosurgery, Director of the Cerebral Blood Flow Reconstruction Center, President of the National Regional Medical Center and Xuanwu Hospital Jinan Hospital. He is also the editor-in-chief of the Chinese Journal of Cerebrovascular Diseases, deputy chairman of the Neurointerventional Committee of the Chinese Medical Doctor Association, chairman of the Neurointerventional Committee of the National Health Commission Continuing Education Center, chairman of the National Health Commission Brain Prevention Committee Ischemic Stroke Surgery Committee, deputy chairman of the National Health Commission Brain Prevention Committee Ischemic Stroke Intervention Committee, and vice president of the Beijing Interventional Medicine Association. He graduated from Shandong Medical University and successively studied under Professor Zhu Shugan and Professor Ling Feng, obtaining a master's degree and a doctorate in neurosurgery. He also completed postdoctoral research at Peking University under the guidance of Professor Bao Shengde. He specializes in the surgical and interventional treatment of ischemic cerebrovascular disease, and was the first in the world to carry out innovative surgeries such as combined surgery for the treatment of carotid artery occlusion and vertebral artery occlusion, as well as drug-coated balloon treatment for vertebral artery stenosis. He has also led the Cerebrovascular Reconstruction Center of Xuanwu Hospital in in-depth research in this field, and has also long emphasized education and training, training a large number of highly qualified doctors in China.
Any use of this site constitutes your agreement to the Terms and Conditions and Privacy Policy linked below.
A single copy of these materials may be reprinted for noncommercial personal use only. "China-INI," "chinaini.org" are trademarks of China International Neuroscience Institute.
© 2008-2021 China International Neuroscience Institute (China-INI). All rights reserved.