NTRODUCTION
Primary central nervous system lymphoma (PCNSL) is a subtype of non-Hodgkin lymphoma (NHL) restricted to the brain, spinal cord, cerebrospinal fluid (CSF), and/or eyes. PCNSL is a rare but well-described central nervous system (CNS) malignancy with distinct treatment and prognostic implications compared with other brain tumors.
Historically, PCNSL was treated primarily with whole brain radiation therapy (WBRT), similar to gliomas and other primary brain tumors. Treatment has evolved over the years, however, and initial treatment now consists of polychemotherapy with high-dose methotrexate-based regimens, which are distinct from those used to treat systemic NHL.
ACUTE SYMPTOM MANAGEMENT
Patients with PCNSL may present with acute neurologic manifestations of the disease, including altered mental status, weakness, headache, seizures, and deterioration of performance status. After diagnostic biopsy has been obtained, an initial course of glucocorticoids, when indicated, often results in significant improvement in symptoms and performance status prior to initiating definitive chemotherapy.
A typical regimen of glucocorticoids for moderate to severe symptoms due to central nervous system (CNS) disease is dexamethasone 8 to 16 mg daily, oral or intravenous (IV), in one or two divided doses. Lower doses can be used for milder symptoms. Maximal symptomatic effects are typically seen within two to three days. Once lymphoma treatment is initiated, glucocorticoids should be tapered gradually to the lowest effective dose to minimize steroid toxicities. Most patients with responding disease are able to be weaned off steroids completely by the second or third cycle of induction chemotherapy.
Pneumocystis pneumonia prophylaxis is particularly important in patients receiving glucocorticoids and concomitant chemotherapy. Due to overlapping effects on folate metabolism, we avoid using trimethoprim-sulfamethoxazole in patients receiving high-dose methotrexate. Alternative prophylactic regimens are reviewed separately.
●Pretreatment evaluation – Patients with newly diagnosed primary central nervous system lymphoma (PCNSL) require an extent of disease evaluation as well as pretreatment laboratories and functional assessment to determine fitness for high-dose methotrexate-based chemotherapy.
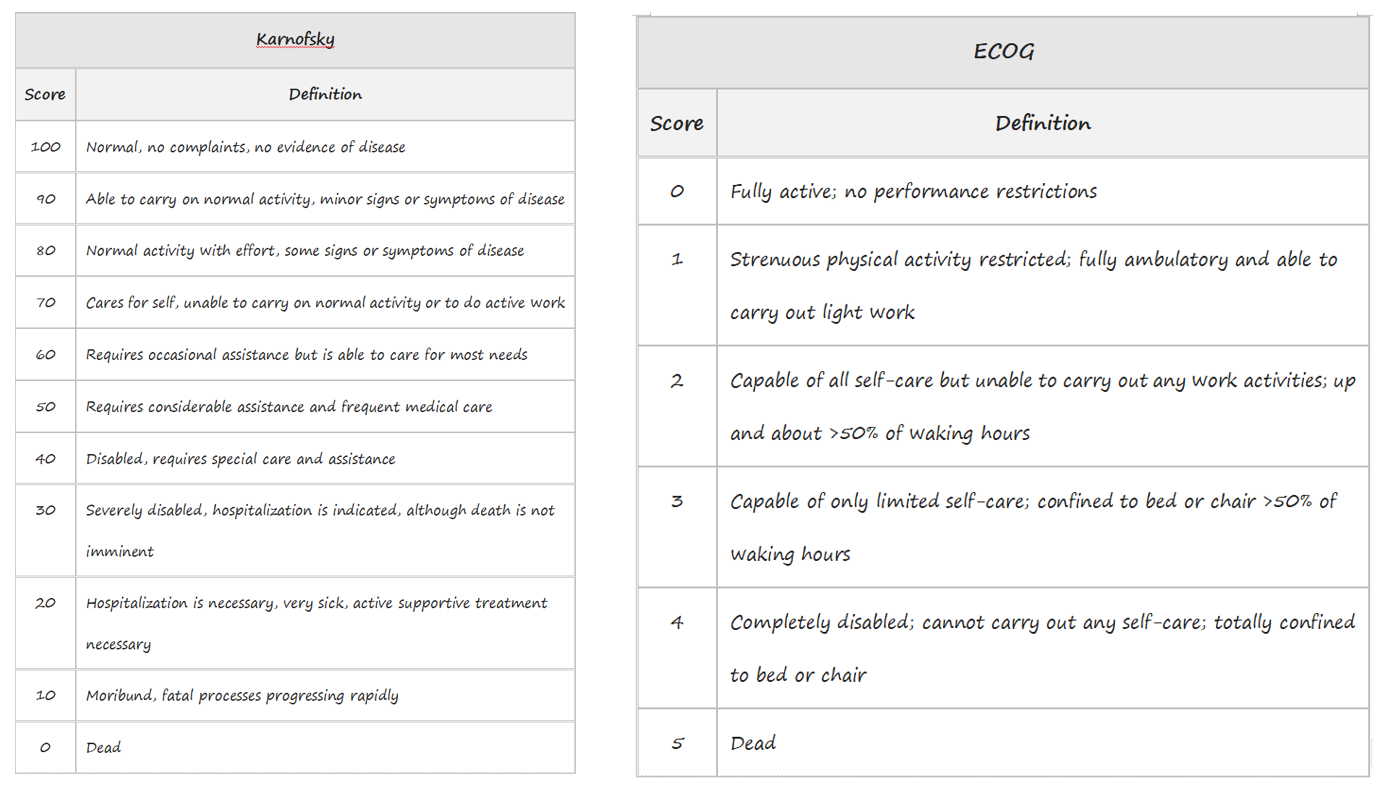
Age and performance status are the strongest independent predictors of overall survival (OS) in patients with PCNSL. Two prognostic scoring systems developed specifically for PCNSL are available to assist in counseling and treatment planning.
Karnofsky and Eastern Cooperative Oncology Group (ECOG) performance status measures
●Induction chemotherapy – For patients with adequate fitness and kidney function, we recommend a high-dose methotrexate-based combination regimen rather than high-dose methotrexate alone or primary radiation therapy. We suggest including rituximab in induction regimens, although evidence is mixed.
Few trials have compared different chemotherapy combination regimens; objective response (OR) rates for most regimens are similar. For most patients, we suggest either MTR (methotrexate at 8 g/m2, temozolomide, and rituximab) or R-MPV (rituximab, methotrexate at 3.5 g/m2, procarbazine, and vincristine). The MATRix regimen is also reasonable to consider in younger, fit adults.
Treatment options are limited for patients who are not eligible for high-dose methotrexate induction therapy due to low performance status or organ dysfunction. Importantly, patients ≥65 years of age are able to tolerate treatment with high-dose methotrexate, and it is kidney function and functional status rather than age alone that should guide treatment decisions.
●Response assessment – Brain MRI with contrast should be performed at regular intervals (eg, every two to four doses of methotrexate) during induction. We aim for a complete response (CR) before proceeding with consolidation therapy, up to a usual maximum of eight doses of high-dose methotrexate.
Experts vary in the approach to patients with a partial response (PR) to induction methotrexate. For patients with clinical and radiographic improvement yet residual enhancing disease on MRI despite up to eight doses of high-dose methotrexate, we most often give a cycle of high-dose cytarabine and, for patients with stable disease or better after cytarabine, proceed with further consolidation. An alternative for transplant-eligible patients with a PR is to proceed directly to high-dose chemotherapy.
Patients with progression during induction or a best response of stable disease are considered to have primary refractory disease and have a poor prognosis.
●Consolidation in patients with responsive disease – The three options for consolidation in patients who have responded to induction are high-dose chemotherapy with autologous stem cell transplantation (HDC-ASCT), nonmyeloablative chemotherapy alone, and reduced-dose whole brain radiation therapy (WBRT). Few comparative trials have been performed, toxicity profiles vary considerably, and many older adults are not good candidates for any of the three. We engage patients in shared decision-making and encourage participation in clinical trials.
•For most young, fit patients, we offer thiotepa-based HDC-ASCT. Patients should be referred for bone marrow transplantation evaluation early in induction therapy in order to minimize delays between induction and consolidation.
•For most patients up to 75 years of age who are not eligible for or interested in HDC-ASCT, we suggest consolidation with nonmyeloablative chemotherapy (cytarabine with or without etoposide) rather than WBRT or no consolidation.
•A watch-and-wait strategy is appropriate for many patients who are not candidates for consolidation, particularly those who are in CR at the completion of induction. The value of continuing high-dose methotrexate or temozolomide monthly as maintenance therapy is uncertain.
●Relapsed/refractory disease – Treatment of relapsed/refractory PCNSL is individualized, and prognosis is poor. Treatment selection is individualized based on a variety of factors, including patient age, performance status, neurologic status, comorbidities, site of relapse, prior treatment, and duration of prior response.
•Rechallenge with high-dose methotrexate is appropriate in patients who previously responded to therapy and have had a prolonged period of remission (eg, 12 to 24 months or more), and highly select patients may be candidates for thiotepa-based HDC-ASCT as salvage therapy.
•For all other patients, options include systemic therapies such as ibrutinib or lenalidomide, radiation therapy, and participation in clinical trials with agents such as chimeric antigen receptor T (CAR-T) cells.
You can find professional doctors and experts about this disease here for your further consultation and treatment.
Any use of this site constitutes your agreement to the Terms and Conditions and Privacy Policy linked below.
A single copy of these materials may be reprinted for noncommercial personal use only. "China-INI," "chinaini.org" are trademarks of China International Neuroscience Institute.
© 2008-2021 China International Neuroscience Institute (China-INI). All rights reserved.